1. NITROUS OXIDE
Nitrous oxide. N2O. A colourless gas with a faint smell and a slightly sweetish taste.
Putney, London
There were more than five million molecules of laughing gas inside me at the moment I was conceived[1]. This does not make me in any way remarkable - it was the same for you.
Let me explain: there is a trace of nitrous oxide, or ‘laughing gas’[2] as it is often called, in the air we breathe each day. Its concentration is roughly three parts in ten million. We know from the analysis of air bubbles inside glaciers that this has been so for at least the last three thousand years[3]. It follows that all of us have laughing gas dissolved within us throughout our lives, as had our mothers and their mothers too.
(My wife, Isabel, says that you have to be a scientist to understand this, and a screwball to think of it in the first place.)
Saturday the 16th of June was a fine day. The sun shone brilliantly in a cloudless sky. By mid-morning my mother was well on in labour, her third in five years, and though she was coping well enough she accepted the gas-and-oxygen which was offered to her.
When her next contraction started she held the mask tightly to her face and took a deep breath. In this way she caused the pressure within the machine to fall, so allowing valves to open and nitrous oxide and oxygen to flow. The mixture of gases she now breathed contained only 10% oxygen[1] which is less than half that in the air. I was not particularly bothered by this because my haemoglobin, like that of all babies, was designed to handle low oxygen pressures, and in any case the flow of blood through my placenta was greatly reduced during the contraction.
When at last her uterus relaxed, the blood flow was restored and by simple diffusion across my placenta I was exposed to pharmacological levels[2] of nitrous oxide even before I was born.
Our house and its close neighbours in the Upper Richmond Rd had been built by Admiral Nelson for his captains to live in when they retired. My mother had told me this, so I knew that it must be true[1a]. I liked the idea immensely for she had also told me that Admiral Nelson had been very famous, and I was sure that I too would be famous when I grew up.
One fine summer’s day I spent most of the morning playing in the garden. In the shed behind the garage I found some sheets of asbestos. These proved enormous fun, for I discovered that if I went at them with a hacksaw I could produce great clouds of white fluff which floated in the air like candy floss and which could be blown around most pleasingly[1]. There were also lots of beautiful snails in the garden, particularly amongst the spinach plants. I liked to get four or five of them lined up at the edge of the crazy paving that surrounded the back of the house and watch them as they travelled slowly over the stones, leaving trails of shiny mucus behind them.
Just before lunchtime I went indoors and upstairs to the playroom. I hoped lunch would not be too long as I was very hungry, but my mother had said that there was one more patient to come and our dining room was where the patients waited. It did seem strange to me that people came from far and wide to this house to get their teeth ‘seen to’, whatever that meant. From the playroom I could peep out of the window and watch them come and go without them knowing anything about it.
Here was someone coming down the drive now, in a hurry, a great big man with a brown hat and a red face. I heard the bell ring and a few moments later the bright yellow front door was opened, and then closed with a thud.
Now a blue car was turning through the gate. Who could this be? Then I recognised the man inside the car. It was the doctor who had looked down my throat and into my ears last week when I had been unwell. He, too, was let in through the yellow front door.
I watched the busy road beyond the garden, which I could see over the top of the brick wall and through the gate. There were lots of cars, and three red double-decker buses. I liked the buses. They seemed friendly things, though why I didn’t know. Perhaps it was because the passengers on the top deck were closer to me than the people in the cars. I waved to them, but no-one waved back.
Suddenly I heard a most unusual noise coming from downstairs. At first I could not think what it was, but then I realised that it was someone roaring with laughter. Not just ordinary laughter, but great noisy bellows that reverberated through the whole house.
I ran to the top of the stairs in amazement. What on earth was happening?
The loud laughter continued for a few more seconds and then there was some shouting, and then more laughter but quieter than before.
I crept down the stairs. By the time I got to the bottom I could only hear voices talking normally, though I could not make out what was being said as the surgery door was very thick.
I tiptoed quietly through the hallway, turned the corner and walked quickly to the kitchen.
‘Mummy, Mummy, why was that man laughing like that?’
‘He was having a tooth out, dear, and the doctor was giving him some gas so that it wouldn’t hurt. Sometimes people do laugh[2] like that, but not very often, I must say, even though they call it ‘laughing gas’.’
This answer satisfied me for the moment. Already there was something more important on my mind.
‘Mummy, what are we having for lunch?’ Show notes
Brimfield, Herefordshire
‘Mummy, my tooth hurts.’
‘Does it, dear?’ said my mother. She continued rolling out her pastry.
I was disappointed by this rather casual response, but decided not to pursue the matter further at that moment.
‘Can I have the pastry bits you cut off?
‘Yes, dear.’
She carefully placed the thin sheet of pastry over the top of the plum pie and trimmed the edges with a knife.
I gathered the trimmings into a ball and started to roll it out as I had seen my mother do.
‘You have to spread a little flour on the table, John, before you do that, or the pastry will stick to it. Look, I’ll show you. What would you like to put in it?’
‘Strawberry jam’, I replied, my mouth watering in anticipation.
Soon the big plum pie and my small jam one were in the oven, together with a few twists of pastry mixed with sultanas and dusted with sugar on the outside. Minutes later a delicious smell filled the kitchen. I waited impatiently for the pies to cook. When at last my mother took them out of the oven they looked quite marvellous, especially the one that was mine.
‘Mummy, can I eat it now?’
‘Wait a few minutes for it to cool or you’ll burn your mouth on the hot jam,’ my mother warned.
I watched the pie longingly for a minute or so and then I gingerly touched the crisp pastry. It was still too hot to pick up.
‘You must be patient, John.’
Eventually the moment of tasting arrived. The pastry was a bit hard but the jam was lovely - lovely, that is, until it found the hole in my tooth. Oh, how it hurt! No wonder that I yelled and burst into tears.
* * *
The dentist in Ludlow was quite clear about it.
‘That tooth will have to come out, I’m afraid. It is too rotten to fill, and it will only give more trouble if we leave it. The doctor is coming for a gas session to-morrow at twelve. Could you bring him back then?’
My mother had hesitated, wishing her dentist husband was not so far away, but there was a war on, and he was in London while we were miles away in a little village in the country.
‘Yes,’ she said, ‘I’ll bring him at twelve.’
So here I was, hungry and a bit frightened, fidgeting in my seat and trying to pretend that I was not worried.
There was another small boy, and a large plump girl, waiting with me. The lady in the white coat, who had shown us into the room when we had arrived, now came back, and said to the girl
‘Come along with me, Anne. The dentist will see you now,’ and off she went.
I wondered what was happening the other side of the door. My mother had told me that the doctor was ‘a very nice man’ and that he would ‘get you to breathe the gas, and you will just drift away to sleep for a few moments so that they can take your tooth out.’
She had said also the tooth would be worth sixpence once it was out. I had just started to plan what I would do with the money, when the door opened again.
‘John, come along with me. There’s a good boy.’
I looked at my mother. She patted me gently on the arm.
‘Just go with the lady, dear. I’ll wait here till you come back.’
So off I went, all alone, out through the door and into the next room.
‘Hello, John,’ said the dentist whom I had seen the day before.
‘Hello, John,’ said the tall man standing next to him.
I said nothing. I could feel a fearful sense of panic creeping over me. Somehow I managed to control it, burying it deep down inside me so that it didn’t burst out in a flood of tears.
‘Come and sit in this chair, John. That’s right. I’m going to put this belt across your lap, so that you don’t slip. There that’s it. Now open your mouth.’
I opened my mouth.
‘A bit wider. That’s better. Just bite on this for me.’
I felt something being pushed between my left back teeth. It stretched my mouth horribly.
‘I’m going to pop this over your nose, and I want you to breathe in and out quietly. There’s a good boy.’
He put his hand over my mouth, so that I had to breathe through my nose. The gas had a strong rubbery smell that I did not like at all. I could feel my heart pounding and I felt pale and cold. Then, quite suddenly, there was a buzzing and whirring in my ears.
‘John, John, wake up. It’s all over. You’ve had a lovely sleep, and your tooth is out.’
The voice seemed far, far away, distant and unreal.
‘Wake up, John. Your tooth is out. Just spit into this bowl. That’s right, spit again.’
So I spat, as I had been told, and opened my eyes and looked up at the blurred faces in front of me. My head was spinning and I felt weak and sick.
‘Hello, John. It’s all over. You’ve done very well. Just take a deep breath and you’ll be fine.’
My mouth was full of salty water. I spat again into the bowl, but some of the bloody saliva trickled down my chin on to a towel that had been put round my neck, though I didn’t remember when. I let my tongue wander around my mouth till it found the hole where the tooth had been. I was amazed how big it was. Surely one little tooth hadn’t filled that huge space in my gum.
‘You’ve done very well, John,’ said the tall man, ‘I’ll tell your mother what a good boy you have been. Are you wide awake now?’
I nodded my head briefly but stopped at once as it made me feel dizzy. Then a wave of nausea swept over me and I vomited[1]. How, I wondered, could they ever have called it ‘laughing gas’?
Epsom, Surrey
I enjoyed chemistry lessons. You never quite knew what would happen next - unless, of course, you were the person who set it in motion. It was always very amusing when somebody connected one of the gas taps to one of the water taps and turned them both on for just a moment so that a small amount of water got into the gas pipe. All the Bunsen burners would go out one after another as the water travelled down the line. If the deed was carried out skilfully it was impossible for the master to prove exactly who had done it, even though he might have his suspicions.
Then there was nitrogen tri-iodide, which was even more fun. You could make it by dissolving iodine crystals in concentrated ammonia. It was stable while it was still wet, but as it dried it became delightfully unstable. If you sprinkled it surreptitiously over the floor it would dry out and then disintegrate with a bang when people walked on it. Splendid stuff!
Another good trick was to put some hydrochloric acid in the open gully that ran under the sinks on one side of the room and some sodium sulphide in the one opposite. The two gullies joined together at the far end of the room just before disappearing down the drain. You could gently wash the chemicals along until they met, when they would react to produce hydrogen sulphide gas, which was the stuff that made rotten eggs smell so horrible. Terribly amusing!
It was also very exciting to put a glowing spill in a beaker full of oxygen and watch the spill burst into flame. I told my father about this at lunch one day during the school holidays.
‘Oxygen is not the only gas that can do that, you know,’ my father said.
‘Isn’t it?’, I asked rather doubtfully.
‘No, it isn’t. Nitrous oxide will do it too[1]. You know, the gas we use to take out teeth. I’ll show you when we’ve finished lunch.’
I wondered whether he was not mistaken, but he did sound very sure about it.
The meal ended with a lovely Apple Charlotte, which was one of my favourite puddings. I had two large helpings and asked for a third, but without success - mother liked to have some ‘left overs’ to put in the fridge just in case they should come in handy to-morrow or the next day.
‘Ten across. Seven letters. C, five letters, E,’ said my father, lighting yet another cigarette. Can the headgear do it? Yes! What can that be?’
The crossword was always a source of great entertainment both during and after lunch, though it wasn’t often that I came up with the answer before my father or mother did, except for the occasional anagram or something factual that I knew from science lessons at school.
‘Let’s go downstairs now, John, and I’ll show you how nitrous oxide will light a glowing spill. Have you got an empty jam jar we could have, Ethel, please?’
‘You’ll be careful, Jack, won’t you? I don’t want you blowing yourselves up.’
‘We’ll be very careful. Don’t worry, dear.’
So we went down to the surgery with an empty jam jar, and my father turned on a blue cylinder on the gas machine with a special spanner that was tied to it by a piece of string. Then he moved a lever on top of the machine and I could hear the hiss of gas escaping from the tube at the front.
‘Hold the jar so that the gas blows into it, John. That’s right. Leave it there for a while so that all the air is washed out. Now put your hand over the mouth of the jar so that the gas can’t get out. Good.’
He turned the gas off again.
‘You’ll have to stay like that while I get a spill from the kitchen.’
‘OK, Dad.’
It seemed like ages before he came back with a yellow wooden spill taken from the small pot that was kept next to the cooker.
‘I’ll light it and let it burn for a moment. Now I’ll blow it out. There, that’s grand, it’s glowing nicely at the end. Put the jar down on the table and take your hand off.’
As I took my hand away from the top of the jar my father quickly popped the glowing spill into the middle of the jar. The spill immediately burst into flame again, momentarily burning more brightly than before. He lifted it out straightaway.
‘It will go out anyway if we leave it in the jar. It uses up the oxygen in the nitrous oxide and leaves the nitrogen, which won’t support combustion. Also if it gets too hot it will crack the glass.’
‘Gosh, that was great, Dad. It really did burn in the gas, didn’t it? Wait till I tell them at school.’
The doorbell rang.
‘That’ll be my next patient. Would you take the jam jar back to Mum, please.’
‘Yes, Dad, and thanks for showing me.’
Guy’s Hospital, London
Eyes, Skins and Anaesthetics... that certainly was a funny mixture for my next three months as a medical student, but I enjoyed it immensely.
The consultant dermatologist took his teaching duties very seriously and could be relied upon to be both entertaining and informative. Unfortunately he went about it in a very inconsiderate manner as far as the patients were concerned. One of the students would take a history from the first patient, make a careful examination and then present the case to the consultant and the other students. He would demonstrate the physical signs he had elicited and offer suggestions as to the diagnosis, if he could. Then the consultant would ask questions of the group and discuss the answers they gave him. He would write all over the blackboard and quite indefatigably fill up an hour or more with a splendidly extrovert discourse on a huge variety of subjects. I repeatedly found myself embarrassed by the thought of the patients waiting outside, to say nothing of the patient in the room. Still at least he got to listen to the lecture with the students. Some of it had to be of interest even to a layman. But those poor people waiting outside! It was one thing to be kept waiting because there were lots of other patients to be seen, but to sit there totally ignored while the students had an hour’s lecture - well, that was another story. When it seemed that he would never finish his talk, let alone the outpatients, the consultant would suddenly wind it up and rattle through the rest of the patients in ten or fifteen minutes. If only he had done it the other way round, seeing the patients quickly first and talking to the students afterwards when the real work was over, how much better it would have been.
The eyes part of the course was a strange mixture. It was so sad to see people who were losing their sight. I did not know how they coped with it; yet they were often so brave. In complete contrast, how wonderful it was when a simple operation, like cataract extraction, restored someone’s vision to them. The routine eye testing was quite interesting at first though it soon became tedious just watching for we never got the chance to carry out any of the tests themselves.
The anaesthetic part of the three months was great fun. Here, for the very first time as a medical student, I felt that I was involved in a practical way with the patients. During my first year at Guy’s I had learnt to take histories and examine chests and abdomen and feet, and many other things besides, but somehow it all seemed a bit unreal. Nothing that I did actually seemed to matter. No, that wasn’t true. All the blood samples that I took for tests in the laboratory were important, but I felt that most of the other things I did were to help me learn rather than to help the patients.
During my time with the anaesthetic department I not only learnt how to maintain an airway in an unconscious person, I actually did it. I also put needles into veins, injected drugs that sent people to sleep, and put tubes down their throats and into their tracheas. Exciting stuff!
One particular day we talked about the cylinders on the anaesthetic machine. The cylinders that were black with white shoulders contained oxygen; the blue ones nitrous oxide.
‘Why is that nitrous oxide cylinder all wet on the outside, while the other one is quite dry?’ I asked the anaesthetist who was teaching me. He was a small wiry enthusiastic man, who had written an amazing book on how anaesthetics work[1].
‘Well, the wet one is the one we are using at the moment and the dry one is the spare,’ came the reply. ‘Nitrous oxide liquefies under pressure, and a full cylinder has liquid in it right up to the shoulder, here, though there is some gas left at the top of the cylinder. When we open the valve to let gas out some of the liquid nitrous oxide underneath will evaporate to replace it. The cylinder gets cold because as it evaporates it absorbs heat. The water you see on the outside is only like dew settling on the grass at night-time when the temperature drops. If the operation goes on long enough the water will get so cold that it will turn to ice, just like dew turns into frost.’
I was fascinated.
‘How cold does the cylinder have to get before the water starts to collect on it?’ I asked.
‘That depends on how wet the air in the room is. If it is very dry then it will need to be much colder than if it is damp. As it happens we like to keep the air in the theatre quite moist so that there won’t be too much static electricity around. That way there won’t be any sparks to cause explosions. Lots of anaesthetics are inflammable, you know.’
‘How long does a cylinder last?’
‘Well, a full cylinder this size will last about five hours if you use it at six litres a minute, but of course you don’t always start off with a full one.’
‘How do you know when to change over the cylinders? Is it by watching the pressure gauge.’
‘Well, yes, but it isn’t quite as simple as that. You see the pressure falls at first because the temperature falls. If it wasn’t for that, the pressure would stay steady as long as there was some liquid left in the cylinder. When the last drop of liquid evaporates there isn’t really much gas left and the pressure falls rapidly as the gas gets used up. You have to watch closely or it runs out when you’re not looking. You could weigh the cylinder at the start of the day and work out how full it is that way, as the weight of the empty cylinder is stamped on it. see here it is.. but nobody ever does. I just tap it like this and get an idea of the liquid level by the note it makes, and anyway someone has written on it with chalk so that we know how many hours it’s been in use without doing anything.’
‘When was nitrous oxide first used?’ I asked.
‘It was Humphry Davy - you know, the man who invented the lamp that coal miners take down mines - who found that it cured his toothache when he breathed it. In 1799, I think it was. He suggested that it might relieve pain in surgical operations[2], but no-one actually tried it out for years. That’s amazing, isn’t it? But in 1844 there was a dentist called Horace Wells who happened to watch a demonstration of its effects during a lecture-demonstration in Hartford, Connecticut. He noticed that a young man banged and bruised his shin without it hurting, at least not until the effects of the gas wore off. So the next day, which was December 11th 1844, he got someone to take out one of his own teeth while he breathed it. It worked splendidly. Unfortunately when he tried to do it at the Massachusetts General Hospital in Boston it wasn’t very successful and the students who were watching jeered, hissed and cried out ‘Humbug!’. Poor Wells, he deserved better than he got. He committed suicide in the end. He was still only 33 years old.’
‘That’s terrible. What happened?’
‘Well, ether came along in 1846 - that’s a story in itself [3]. It wasn’t till years later that nitrous oxide came into general use. Wells gave up dentistry, got himself into trouble by throwing acid at a prostitute and was put in prison. Really he deserved a medal for putting his original observation to clinical trial which was more than Humphry Davy ever did.’
Humphry Davy In Bristol c.1800, from the City Museum
Horace Wells, from the Clendenning Library
Our conversation was interrupted by the arrival of the next patient who was soon put off to sleep with an injection of thiopentone.
‘Thiopentone was introduced as an intravenous induction agent in 1934,’ I was told.
Oh, I thought, that’s the year that I was born!
Half an hour later I found myself temporarily alone watching the patient and the anaesthetic machine while the anaesthetist got the drugs ready for the next patient and discussed with another doctor a problem case that was due later in the morning. I looked carefully at the lady and saw that she was warm, dry and pink and that her respirations were deep, easy and regular. I put a finger on her pulse and noted that it was full and strong and regular. The oxygen was set at two litres a minute and the nitrous oxide at six litres a minute. I glanced at the cylinders and saw that the bottom of the blue one was covered thickly with ice, while the top half was wet with water. I looked at the dial. It was reading nearly zero pressure. It must be almost empty! I knew exactly what to do. I took the cylinder key from the back of the machine where it was hanging by a loop of string. I first turned off the cylinder that was nearly empty and then I turned on the new cylinder, as I had been taught. The needle of the pressure gauge swung round to read 750 pounds per square inch. It was a moment of great satisfaction.
* * *
Later that month I attended a ‘gas’ session in the dental department. It was fascinating. The anaesthetic machine was very similar to the one in my father’s surgery at home. I watched a couple of small children being persuaded to ‘sniff the nice gas’ as they sat in the dental chair; a few moments later they were having teeth wrenched from their mouths by the dentist. Then I was invited to administer the gas to the next patient, who was a boy of about fourteen. I was shown how to pop the small mask over his nose, how to fix the tubing at the back of his head and how to support his chin and push it forwards. We started off with a few breaths of pure nitrous oxide, and then added 10% oxygen for a few more breaths before increasing it to 15%. The boy appeared to lose consciousness very quickly, and very soon his tooth was also in the bucket on the floor. It was wonderful, terrifying, fun, but there did seem to be rather too many things to think about all at once.
The three cases still left to be done were not going to be quick ‘smash and grab’ affairs as the others had been, since there were several difficult teeth to be removed from each mouth. The anaesthetist explained to me that for these longer cases he preferred not to reduce the oxygen below 20%, but to add some Trilene [see chapter 5] to the gas mixture instead. It worked very well.
When I got home that evening I got my father’s old book on anaesthetics[4] off the shelf and read the chapter on Signs of Nitrous Oxide Anaesthesia. The first paragraph said:
Almost every anaesthetic can reduce a patient to the point of death, even though he is abundantly supplied with oxygen. The one notable exception, of particular interest in dentistry, is nitrous oxide...
That sounded pretty safe.
... but it is often difficult to subdue him sufficiently to allow even a minor operation to be performed.
But that did not sound very satisfactory! Even if it was a safe gas, you would need it to be strong enough to do the job, wouldn’t you? It was no wonder that they reduced the oxygen a bit to give it some oomph. However, a little further on I saw there was a note of caution about this:
It is essential to understand, during the administration of nitrous oxide, which signs indicate that the patient is (i) adequately anaesthetised, and (ii) dangerously asphyxiated.
Well, that certainly seemed a good idea. You would not want patients to get ‘dangerously asphyxiated’, would you? Next it said:
The chief signs of nitrous oxide-oxygen anaesthesia in order of importance are alteration in the respiratory rhythm, muscular signs, eye signs and colour changes.
Reading on it became quite clear why the respiratory signs were the most important. If the patient was not breathing regularly and through his nose, then he was not deep enough. However this was something of a ‘negative sign’ as co-operative patients might do it even though they were too light:
When such a patient is in the analgesic stage the respirations may lead the anaesthetist to think that anaesthesia has been reached, and he may allow the dentist to begin work.... It is obviously undesirable for extractions to be performed at this stage, but this is not a grave mistake if the patient is sufficiently placid, because, as a rule, when he recovers he merely remarks that he was aware of the removal of the tooth.
Amazing! I guessed that it would have been be a different matter if the patient had felt pain, but perhaps it would not be so bad to know your tooth was being pulled if it did not hurt. After all that was what happened when a local anaesthetic was used.
I skipped on to the section on muscle signs:
Since muscular relaxation results from deep anaesthesia, it is seldom a feature of nitrous-oxide anaesthesia. Fortunately relaxation is not essential for extractions, as the mouth is propped open beforehand.
The memory of the dentist thrusting a prop between my teeth when I was a young child came rushing back to me. How revolting the rubber had tasted, and how unpleasantly it had stretched my mouth!
If the oxygen intake is sharply reduced the tone normally present in muscle is readily superseded by spasmodic contraction. This spasm occurs first in the small muscles of the tongue,...
Small muscles of the tongue? I had always thought of the tongue as just one big muscle!
... but is here rarely noticed, and its early manifestations can be more conveniently observed in the eye, where spasm of the intrinsic muscles pulls the eye out of centre.
Sounded nasty, didn’t it?
Twitching and spasmodic contractions of the larger muscles of the arms and legs follow.
That sounded even worse!
Later there may be opisthotonus...
Opisthotonus? What a lovely word! I knew that it described spasm of the neck and back muscles so that the body became arched backwards as though the patient had been poisoned with strychnine.
... and inspiratory crowing caused by spasm of the adductor muscles of the larynx.
Crowing? Yes, I remembered a patient the previous week who had had some laryngeal spasm in the middle of an operation on his piles; the anaesthetist had described it as ‘crowing’. I was not sure that it was really a very good description, surely crows crowed during expiration not inspiration, but I could not think of anything better.
If deprivation of oxygen is continued still further, this spasm gives way to complete relaxation, quickly followed by death,
What a terrible thing that would be! I moved on to the section about eye signs:
Eye signs are helpful to the beginner, but the experienced anaesthetist comes to use them less and less until finally he rarely, if ever, inspects the eye.
Over the page there were some interesting pictures showing an anaesthetist pulling open the eyelids of his patient to see if the if the pupil was central or if was fixed eccentrically.
If the eye appears to be able to focus, unconsciousness has not been reached.
Appears to be able to focus? That seemed a bit vague. I wondered what they meant exactly. Not just the pupil contracting, surely, or they would have said so. I looked at figure 18, but was not much the wiser.
The eye soon loses this look of intelligence and it is often possible to tell, solely by watching the eye, the time at which consciousness is lost.
That seemed remarkable to me. I would have to ask someone to show me this when I was next in the operating theatre.
Later the eyeball develops a quick, horizontal movement, the rapidity and excursion of which diminish with deepening anaesthesia. The characteristic eye movements of nitrous oxide anaesthesia are manifestations of muscular spasm due to oxygen lack.
Oxygen lack, again! I skipped on to the next section, which was about colour changes:
Cyanosis, as a sign of anaesthesia, is unreliable.
Cyanosis. Wasn’t that also a splendid word? I remembered looking it up once in the dictionary when I was learning physiology at Cambridge. The word came from the colour of the plant pigment cyanin, which is blue in the cornflower, but red in a rose because of the acid that was in rose petals. Just like litmus paper! It referred here, of course, not to plants, but to the colour of a patient’s skin, which would be blue, or cyanotic, if there was a shortage of oxygen in the blood flowing through it.
There were also some comments about the pulse:
The pulse is of little value as a guide to N2O anaesthesia. Early, it may be quickened from excitement or fear....
That certainly was no surprise! I remembered how frightened I had been in the dentist’s waiting room that day long ago in Ludlow.
.... while in asphyxia it becomes slow, full and bounding. The significance of both may be erroneously interpreted, the former as heart disease, the latter as a reassuring sign. By the time the asphyxial pulse is noticeable, other conspicuous signs indicate that oxygen-lack is excessive. The onset of any cardiac irregularity at this stage is an urgent indication for the administration of oxygen.
This reducing the oxygen to make the nitrous oxide more potent did seem rather dangerous, but it was done every day throughout the country, and my father had watched doctors doing it without any problems since World War I. So it must be all right really, mustn’t it? Of course, my father’s book was 16 years old now, so it might well be out of date. I wondered what a modern textbook[5] would say.
The next day I went to the medical school library. I found a book called Modern Practice in Anaesthesia that had been published in 1954, so clearly it was the latest edition. It had been edited by a Dr Frankis Evans from St Bartholomew’s Hospital. I guessed he must be the man who designed the indwelling intravenous needle which we had used in the operating theatre the day before.
This book had a section on Nitrous Oxide and Asphyxia, which made interesting reading:
The statement by Haldane (1922) that ‘anoxaemia not only stops the machinery but wrecks the machine’ is as applicable to anaesthesia with nitrous oxide as it is to any other clinical condition.
It went on to discuss and condemn what was called ‘secondary saturation’, which apparently was a technique recommended in America. In this the patient was given nitrous oxide alone until respiration ceased. By then the patient would be deep blue, his pupils fixed and dilated and his pulse weak and irregular. The lungs were then forcibly inflated with a high percentage of oxygen and the pulse would improve, the colour become pink, the pupils constrict and the respiration return. After this the muscles apparently became relaxed, as a result of shock induced by asphyxia.
Further down the page it said:
It is clear, therefore, that the only method of avoiding hypoxia is by maintaining scarlet blood.
Scarlet blood? What a splendid description! It sounded like something from Hollywood. Anyway, it seemed clear enough that reduction of oxygen was no longer recommended.
Imagine my surprise then when I read, a few pages later a clear description of how to give an anaesthetic with nitrous oxide and oxygen that contained the following instructions:
Induction of anaesthesia is best produced by the inhalation of nitrous oxide alone. This results in emptying the lungs and respiratory ‘dead space’ of their contained gases, including the nitrogen content, and in depleting the oxygen stores of the body. By this means a quicker induction may be obtained and a much smoother and more stable anaesthesia is obtained afterwards. As soon as automatic respiration is established, oxygen is added, at first in a small quantity. The mistake most often made by novices is to give too much oxygen at the beginning of anaesthesia, and too little during the later stages. As has already been indicated, cyanosis is to be avoided.
So there it was. Hypoxia was a bad thing, but it was all right in small amounts for brief periods in healthy patients. Clearly, it called for some fine judgement.
Taunton, Somerset
Isabel and I had been at Taunton now for eight weeks. We were firmly settled in our flat at 10 Richmond Rd (what a coincidence that was!), and I was enjoying my new job as Senior House Officer in Anaesthetics very much. I seemed to have picked up the basic skills of airway management and intubation of the trachea quickly enough, but then I had had to, as I had been thrown in at the deep end in a way that I think was totally indefensible when I reflect upon it thirty four years later.
So there I was, inexperienced and unsupervised, anaesthetising for a list of tonsillectomies. In contrast, the surgeon was very senior and experienced - and what a good thing too as it turned out.
The morning had gone rather well considering how relatively new it all was to me. Five small children and ten tonsils removed without any major problems, though there had been a moment or two of private and silent anxiety.
The last patient was a boy of sixteen. Because he was so large I put a tube through his nose and throat and into his trachea[1] to make things easier, though I had managed the smaller children without an endotracheal tube. Ten minutes later the operation was almost finished, the tonsils were in the dish on the instrument trolley and there were just a few bleeding points left to be stopped. I turned the ether off but let the nitrous oxide and the oxygen continue as before.
Soon the last ligature had been tied. The gag that was keeping the patient’s mouth open was loosened a little and the throat checked for bleeding one last time. I turned off the nitrous oxide and turned the flow of oxygen up to six litres a minute.
The surgeon and I waited till we saw the muscles at the back of the throat begin to contract which told us that the reflexes protecting the larynx had returned. I popped a rubber airway into the mouth, took hold of the tube as it emerged from the nostril, and with a flourish pulled it right out, turning the boy onto his left side as I did so.
The boy gave a cough, took two breaths, coughed again and then stopped breathing. I was not really worried at first. I thought there must be some blood or saliva irritating the larynx, causing the vocal cords to shut tightly and making the boy hold his breath. I knew the lungs were full of oxygen, so everything would be all right if the breath-holding did not go on for too long. Half a minute passed. I put my fingers behind the angles of the jaw and pulled forward forcibly, ensuring that the airway was clear and hoping that the painful stimulus would make the boy take a breath. But he didn’t and before long he started to go a dusky blue.
I thought I had best give him some oxygen from the anaesthetic machine so that when he did take a breath at least it would be oxygen rather than air that he took in. I put the mask tightly over his face and turned on the high flow oxygen switch at the top of the machine. The boy was looking very blue indeed by this time. To my great relief he started to breathe again. He’ll go pink in a moment, I thought, any second now he’ll go pink; the oxygen will get to the blood as it passes through the lungs, and he’ll go pink as the blood is pumped by his heart to every part of his body.
To my horror and amazement the boy, who was breathing deeply and rapidly, did not get pink at all. He got more and more blue as every second passed until he looked almost black, though at the same time he began to go pale in patches. What, in God’s name, was happening? What was I to do? He’ll die if I don’t do something!
With a sense of utter panic and total despair welling over me I looked up to see if there was anyone around who could help me. The surgeon, who was looking as anxious as I was, turned and studied the anaesthetic machine.
‘The bobbin is at the top of the nitrous oxide flowmeter,’ he said. ‘You must be giving him nitrous oxide instead of oxygen.’
I looked at the machine. He was right! Then I saw that there were two ‘high flow’ levers, one on each side of the flowmeter panel. I had turned on the one by the nitrous oxide tube and not the one by the oxygen tube. Quickly I changed the positions of the two levers and seconds later the boy had become a wonderful pink colour again. My hand was shaking and a cold sweat was running down my face and dripping from my chin.
‘I thought I had killed him,’ I said.
‘All’s well that’s ends well,’ the surgeon replied, ‘but fancy there being two levers. That seems very dangerous. Of course,’ he added, ‘he would have been all right if you had just let him breathe air instead of trying to give him oxygen. That’s a curious thought, isn’t it?’
We discovered later that the machine I had been using was the only one in the hospital that had a high flow lever for nitrous oxide[2].
We phoned the service engineer and got him to remove it before another crisis could occur.
It was the day before Geoff’s wedding in Rickmansworth. Isabel, four months old Timothy and I were travelling to Putney where we were going to stay for two nights. Timothy was going to stop with his Granny while we went to the wedding on the Saturday. Isabel was eagerly looking forward to a day off, though she was worried that I would not be properly dressed since I had refused to hire a morning suit.
‘I am sure everyone will be in formal clothes,’ she said. ‘You really should get something from Moss Bros., you know. You will feel very silly if you’re the only person in the wrong clothes.’
‘Nobody goes to weddings dressed like that these days, darling, unless they’re part of the family. Anyway, we can’t afford to hire one. But it will be OK, my love, you’ll see.’
‘Well. I hope so.’
We drove on across Salisbury Plain. The little car, an Austin A 30, was a real joy. It was running beautifully on ten volts instead of the normal twelve. I had discovered only the day before that one of the cells in the battery was not working properly, and as I had not got the money for a new battery the mechanic at the garage had put a piece of copper wire across the appropriate terminals to by-pass the fault. I was greatly relieved to find it working so well.
‘Shall we stop at the Linga-Longa restaurant for a cup of tea when we get there?’ I asked.
‘No. I think we had better press on while Timothy is sleeping. We’ve a long way to go. Anyway I don’t fancy the Linga-Longa. The service was very bad the last time we stopped there.’
‘OK, but my mouth is very dry. Have you got a peppermint handy?’
I knew that she had, and I was hoping that the mention of peppermints would put something else into her mind.
‘Yes, I’ve got one. Here you are. I think I’ll have a cigarette as well. Would you like one? I’ll light it for you if you like.’
The ruse had been successful! Ever since she had become a nurse Isabel had always had a peppermint after she smoked a cigarette, so that she would not breathe tobacco all over the patients. I had been smoking heavily throughout the journey from Taunton and I had not wanted to light another one on my own in case Isabel thought I was smoking too much. This way it had become her suggestion not mine. Pavlov would have been proud of me!
It was three o’clock before we reached the Upper Richmond Rd and turned into the drive. The white house looked lovely this sunny summer’s afternoon. Nostalgic memories flooded through me as I saw the front door, which was still the bright yellow I remembered as a child.
‘Come on, John. Don’t day-dream.’
Soon we were upstairs in the sitting room and my mother was admiring Timothy, her first grandchild, while Isabel poured out cups of tea.
There was a knock at the door and the receptionist came in.
‘Your father wonders if you could give a gas for him in about half an hour. There is a lady with an abscess who needs a tooth out.’
She paused, waiting for an answer.
I felt the adrenaline surge through me. Here I was, an anaesthetist with ten months experience, who could deal with ill people having major surgery in the middle of the night, and yet I had not given a simple ‘gas’ for a tooth extraction in the dental chair since I was a student at Guy’s, and then I had only done one. I had read all about it, of course, while studying for the Diploma in Anaesthetics examination that I planned to sit in November, and I remembered all about the McKesson gas-and-oxygen machine in the surgery downstairs. As a teenager I had often gone into the surgery and looked at it, so that I knew exactly where all the knobs and switches were, but I had not used a machine like it since I had become an anaesthetist. My father, of course, had had years of experience with such machines. What was I to say? Of course I had to say ‘yes’! Otherwise I would look stupid.
The half-hour turned out to be only twenty minutes, so here I was in the surgery and the patient on the way from the waiting room.
‘I’ve switched the cylinders on,’ my father said.
‘I’ll just check the spare oxygen,’ I replied. Anything to get the feel of the machine before I used it. I remembered clearly that there was only one reducing valve for the two oxygen cylinders so first I turned the ‘in use’ cylinder off and flushed the machine so that the oxygen pressure fell to zero. By this time the patient had come in and was sitting in the chair.
‘I won’t be a moment,’ I said. I turned the full cylinder on, saw the lever on the pressure gauge rise once more. That’s OK, then. Now turn that one off and the first one back on again. Good. Right now put the mixture dial to 0% oxygen and the delivery pressure to 5 mm. Is the nitrous oxide flowing? Yes, but too fast, so reduce the pressure a bit . Good. One last look. Be patient, Dad. Yes, the valve on the nose-piece is open and the machine is close enough to the chair.
The patient was sitting nervously in the chair now with a prop between her back teeth and a bib under her chin.
‘I’m just going to pop this small mask over your nose, Mrs Jones. There that’s it. Just breathe through your nose now. It will smell rather rubbery, I expect. Good, that’s right, not through your mouth but through your nose.’
I pushed the lever across to the 100% nitrous oxide position, put the delivery pressure up a bit and at the same time my father held a gauze pack lightly over her open mouth. She seemed to be going off nicely, I thought, and I could hear the whistle of the expiratory valve at the end of each breath. After a few more seconds I moved the mixture lever to 12% oxygen, put my fingers behind the angles of the jaw and pushed forwards to make certain the airway was clear. I nodded towards my father and looked at the patient’s colour. Just a tinge of blue, perhaps, but nothing to remark about.
‘Thank you, John. That’s it.’
Good Heavens, the tooth was out already! I had just been getting into my stride. I moved the lever to where it said 100% oxygen, which would cut the nitrous oxide off completely and waited for the patient to wake up.
‘Well done, Mrs Jones. Spit into the bowl, please. It’s all over. Your tooth is out.’
Five minutes later I was upstairs again drinking a second cup of tea.
‘How did it go, dear?’
‘Fine, thank you.’
I did not mention that I had been nervous. I made a resolve to get some practice at dental anaesthesia before I came home again. Later my father handed me two pound notes and a florin.
‘Here are two guineas, John. It’s your professional fee. Thanks again.’
‘That’s OK, Dad.’ I replied, and I put the two green notes and the silver coin in my pocket.
Next day there were two hundred guests at the wedding. Apart from myself, only one of the men was not in morning dress. Isabel was very cross with me.
Geoff and Liz went away in style on an elephant their uncle had hired from Billy Smart’s circus.
Royal Infirmary, Bristol
Things were very different in Bristol. People used such small doses of thiopentone that I was amazed that they thought it would work at all. Having just come from Catterick where the fit heavy drinking soldiers often needed five or six hundred milligrams to make sure that they went to sleep it seemed quite astounding to use only fifty milligrams - and they didn’t supplement the nitrous oxide either. In Taunton I had been taught to use ether or trilene or cyclopropane or any one of a number of opiates in addition to nitrous oxide. In Catterick Peter had converted me to the exclusive use of large doses of pethidine, but here it was treated as something almost shameful if you gave the patient anything more than nitrous oxide and some curare. It was very puzzling.
‘Why don’t you use more thiopentone?’, I asked Alan, one of the other registrars. ‘Then the patients would be completely asleep when you put the mask on their face.’
‘Because J.C-B thinks it is anti-analgesic, or antanalgesic, as he calls it.’
‘Antanalgesic?’
‘Yes, he believes that in low concentrations thiopentone counteracts the pain relief produced by morphia[1]. If you give a big dose at the start of the operation, then at the end of it, when the patient wakes up again, you may get low levels of thiopentone persisting that stop morphia working properly. If you only give a small dose at the start, then afterwards the level of thiopentone will be below the antanalgesic concentration. That’s the theory at least. He thinks, too, that during the operation thiopentone possibly may counteract the analgesic effect of nitrous oxide, and certainly it can in the early postoperative period. He reckons that if you give only a small amount of thiopentone then you need less opiates as well. So he uses as little as he can. Anyway large doses depress the patient’s circulation, which can’t be a good thing, and they are perfectly happy to breathe from a mask after a small dose, if you talk to them all the time.’
Well, that certainly was a new way of looking at things. I had noticed that J.C-B. was always talking to the patients, even in the middle of the operation and not just at the end when they were waking up.
‘But you don’t hyperventilate them like the people in Liverpool do, do you?’.
‘No, J.C-B. has a theory about that too. He says that extreme overventilation produces constriction of the blood vessels in the brain and this may cause brain hypoxia[2]. His typical anaesthetic technique is a premed of pethidine 50mgs, Phenergan 25mgs and atropine 1/100 of a grain[3] one and a half hours before the operation, 50mgs thiopentone followed nitrous oxide 66% and oxygen 33% through a facemask; then curare 15mgs, followed by another 15mgs curare two minutes later. He talks to the patients all the way through this period, and gradually takes over their breathing as the muscle relaxant works and they aren’t able to breathe for themselves. After five minutes he pops a laryngoscope into their mouths and a tube into their tracheas. He carries on talking to them through all this - and through the operation as well. At the end of the operation he gives them atropine 1.2 mgs and neostigmine 5mgs to reverse the relaxant, turns the nitrous oxide off, tells them that ‘the operation is all over, Mrs Jones’, and that ‘someone is putting a bandage on your tummy’, and that ‘I am just about to take the tube out of your mouth’. He then says ‘you have done very well, Mrs Jones’, and ‘we are very pleased with you. Are you all right?’. They usually reply ‘yes’ at that time, but ten minutes later they are needing something urgently for pain as the effect of the nitrous oxide has worn off and they haven’t any strong analgesic on board.’
Brilliant stuff, nitrous oxide, but effervescent![4]
There was great excitement at the Maternity Hospital: the Entonox cylinders had arrived at last. Not that they would be any good now for Isabel as she was already delivered of a fine boy whom we had called Charles Jonathan. Anyway, as it happened, she had not felt the need for analgesia during her labour so it did not matter that there had been none of it for her to try. But it was strange to recall that Entonox had been available in Catterick nearly a year earlier than this. I wondered what the reason for the delay in Bristol had been; not that I had been very involved with obstetrics in Catterick, except for Caesarean sections and the occasional forceps delivery for which we had always given a full general anaesthetic.
Since arriving in Bristol I had read an article about Entonox with the intriguing title Nitrous Oxide and Oxygen from a single cylinder[1]. When you considered how differently the two gases behaved when they were compressed individually, the one staying a gas while the other liquefied; it certainly was a curious thing that you could get stable mixtures of them in one cylinder. Furthermore the cylinder would then deliver a constant mixture of nitrous oxide and oxygen independent of emptying, position or storage time, though apparently this was no longer the case if the temperature fell too low. At minus 1.5oC the delivered concentration of oxygen started to rise so that eventually there would be a higher concentration of nitrous oxide in the cylinder if you were to it at that temperature. If you did not use it, which of course you wouldn’t, but rewarmed it instead, the contents did not return to the original state unless you waited seven days or tipped the cylinder upside down three times. The author, a Dr Cole, was clearly very worried about the possible danger of this effect of cooling and thought it unlikely that the Central Midwives Board would approve its use by unsupervised midwives.
Then right at the end of the article there was an addendum drawing attention to a paper[2] in the British Medical Journal which had been published after Dr Cole’s paper had gone to press. In this Dr Tunstall from Aberdeen had contended that 50/50% nitrous oxide/oxygen mixtures were suitable for clinical use on the grounds that:
(a) previously cooled cylinders can be quickly rewarmed by immersing them in water at 42oC for five minutes; (b) their contents can then be returned to normal by
In the event the CMB had approved its use by midwives and here it was in Bristol for them to try.
I was talking to one of the other registrars[3] about it when I suddenly felt a strong urge to try it out on myself to see if it really worked.
‘If I was to breathe Entonox for exactly sixty seconds by the clock, not a moment longer, just to see what it was like and how much of an effect it had, would you think it was very silly of me, and would you stay in the room while I did it?’
‘Well, now,’ he replied, ‘as long as it was done in the spirit of a genuine scientific experiment, and not just for fun, I don’t see why you shouldn’t do it once - but only once. I wouldn’t want to encourage you to become a sniffer.’
‘It’s just that I’m curious,’ I explained. ‘After all in the last six years I must have given tens of thousands of gallons of nitrous oxide to hundreds of different people, and I don’t really have any idea of what it does them. Oh, I did have a tooth out as a child but that was almost certainly gas-and-suffocation rather that gas-and-oxygen. I haven’t got any more patients to-day, and I’m not driving home, so what about it?’
‘OK, go ahead and breathe the stuff if you want to. I don’t see that it could possibly do any harm. Just for one minute though.’
I sat down on a stool, carefully placed so that I could see the clock hanging on the wall. I picked up the mask of the Entonox apparatus and held it closely to my face. I waited for just a brief moment and then as the second hand of the clock swept past twelve I started to breathe steadily in and out.
At first I was only aware of the revolting smell of the rubber tubing but after a few breaths I did notice the sweet taste that nitrous oxide was often described as possessing. After fifteen seconds I realised that something truly pharmacological was happening: objects round about me were getting a bit distant and unreal; the traffic noise from the road outside seemed far away; my head was whoozy and there was a buzzing in my ears and a banging in my head. I’ll never last out a full minute of this, I thought; but I managed to do so. By the time the second hand reached the twelve once more I was markedly intoxicated, slightly nauseated and amazingly light-headed. I took the mask off my face and looked at John who seemed to be dancing before me. I breathed in deeply to get rid of the gas from my lungs. The air in the room seemed fresh and invigorating. Slowly I began to feel more my normal self, though a mild nausea persisted for a full five minutes.
‘Well, I’ll never doubt the power of nitrous oxide again. I am staggered at the effect, and how quickly it came on. I had no idea that such a short exposure would have such an amazing action. It wasn’t the slightest bit pleasant[4]. I don’t think I’ll ever do that again.’
I never have.
I looked at the duty rota and saw that I was down to give the anaesthetics in the X-ray department at the Children’s Hospital on Thursday afternoon. I sought out John Crook and asked him about it.
‘What sort of things will they be doing?’
‘Oh, probably an air encephalogram or two.’
‘I’ve never seen one of those. What exactly happens?’
‘They do a lumbar puncture and take off some of the CSF and inject some air. Then they sit the patient up so that the air gets into the ventricles and shows up on the X-ray and they can see if there is any displacement. As far as the anaesthetic is concerned I think it’s best to give a relaxant and ventilate the patient; that way you can keep the anaesthesia light and the blood pressure doesn’t fall too much when it’s time to sit the patient up. They almost always get a terrible headache afterwards though these days we turn the nitrous oxide off when they get around to injecting the air.’
‘Is that because it will diffuse into the air bubble inside the brain if you don’t? I think I read something about that in Anesthesiology earlier this year.’
‘Yes, that’s right. It was the same clever people from San Francisco who suggested that you should not use nitrous oxide in cases of intestinal obstruction[1] as any gaseous distension would be made much worse and the surgeon might not be able to close the abdomen at the end of the operation. As far as air encephalograms were concerned they showed that there could be a big rise in the CSF pressure if you gave the patient nitrous oxide[2]. I’m not sure that their conclusions were entirely valid because they used the same needle that they had used to inject the air to measure the pressure. This means the hole in the dura was blocked and CSF couldn’t drain through it. When our radiologists do an air encephalogram, they take the needle out and CSF can drain away if the pressure gets high.’
‘Yes, I see what you mean. So the headache they get afterwards might be due to a low pressure once the patient has stopped breathing nitrous oxide and the bubble got smaller again?’
‘I suppose that could be right, but the radiologists always use such large needles for the their lumbar punctures that there must be a big CSF leak even without the effect of the gas.’
‘It sounds horrendous to me. What do you give them instead of the nitrous oxide?’
‘Oh, I usually use a little Trilene; at least that doesn’t lower the blood pressure and it gives plenty of postoperative analgesia. Of course they did suggest that it might be possible to inject nitrous oxide into the CSF instead of air; that way the bubble wouldn’t get any bigger if you gave the patient nitrous oxide to breathe.’
‘I see, but I wonder what would happen to the bubble when you turned the nitrous oxide off. It’s a shame that they can’t make really fine needles so that the hole in the dura isn’t so big.’
‘Perhaps they will one day. Maybe then we’ll start using spinal anaesthetics again.’
‘I doubt it. Not now we have curare.’
(Which only goes to prove how wrong you can be.)
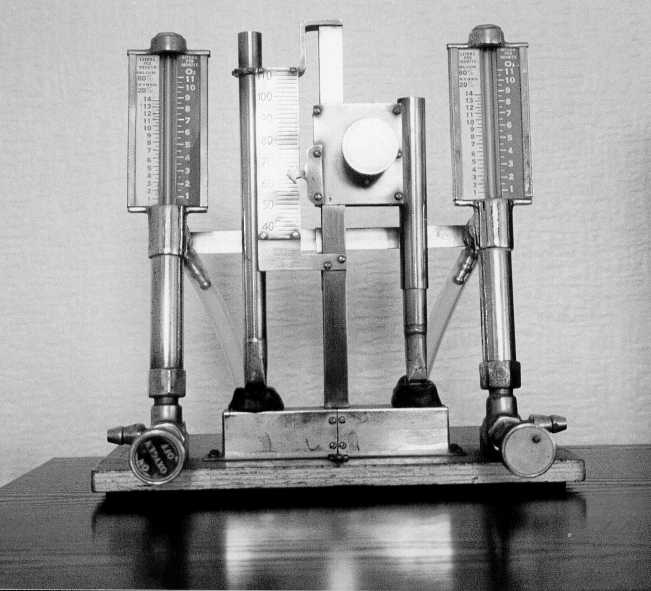
‘What on earth is that? It looks like two miniature organ pipes stuck onto a piece of wood
‘That’s just what it is,’ Graham replied.
‘What’s it for?’
‘It’s for measuring the composition of mixtures of nitrous oxide and oxygen.’
I was in the university department of anaesthetics research laboratory, which was down a short corridor opposite the NHS departmental office. I had recently read a paper by J.C-B describing an apparatus for producing a negative pressure in an anaesthetic circuit during expiration, and I had had the idea that it might work if you just filled the breathing bag with pieces of foam rubber. Now I wanted to record the pressure changes that occurred. Graham would know how to do it, if he could be coaxed into a helpful frame of mind.
‘How does it work?’
‘You blow oxygen through this pipe, and the mixture through that one. Then you turn this knob so that this sleeve moves, and the pipe gets longer or shorter depending which way you turn it. When the two musical notes are exactly the same you can read off the oxygen percentage by looking at this pointer and this scale.’
How ingenious I could see that the pointer was attached to the piece of pipe that moved, while the scale was fixed to the side of the other pipe whose length was constant. That really was clever.
‘Whose invention was that?’ I asked.
‘It was the J.C-B’s idea,’ replied Graham, ‘but I put it together.’
‘I would love to see it working. Can you show me?’
‘Yes. If I connect the oxygen cylinder to this piece of tubing we get a lovely note coming from this pipe. Beautiful, isn’t it? We can make a mixture of nitrous oxide and oxygen with the anaesthetic machine here... like this. If we connect it to the other pipe you can hear the note is quite different. Now turn the knob.’
I reached out my hand and slowly turned it. As the pipe shortened so the note became higher. As it got really close to the first note I could hear a curious warbling noise that was very unpleasant to listen to. It reminded me of two children playing recorders that weren’t quite in tune with each other.
‘That’s called a "beat note",’ said Graham. ‘When the two notes are exactly the same it disappears, so you have a very precise endpoint. There that’s it now.’
Sure enough the unpleasant warble had gone and in its place there was only one pure note coming from the two pipes.
I looked at the pointer and saw that it was opposite the fifty six percent mark on the scale. On a sudden impulse I turned the knob so that the two notes were wildly different and then I slowly turned it back again till the notes were identical once more. Fifty six percent exactly.
‘That’s brilliant,’ I said. ‘I wish I had thought of that.’
I looked at next week’s duty rota to see what I would be doing. I was pleased to see that I was working with J.C-B on Monday morning. That was certain to be interesting.
When Monday arrived I set out early so I would get there in time to find a parking place. I knew from past experience that you needed to be an early bird if you were going to the General Hospital and wanted to be able to park inside the grounds or within a reasonable distance from it.
At a quarter to nine we were all gathered in the gynae theatre suite ready to start the morning’s work.
‘Just a little needle prick Mrs Jones,’ said J.C-B. He took the patient’s left arm, holding it with his thumb and forefinger round her wrist so that the veins became distended. Picking up a syringe with his other hand he thrust the needle into a vein in the reverse direction to that normally used. I knew that J.C-B did it in this way so that he could do it without needing anyone to help him. Eccentric, but effective. (To his intense amusement one of the nurses had written in her pocket notebook that ‘the professor does not like to be interfered with.’) Then he injected 50mgs of thiopentone and withdrew the needle carefully sticking it lengthways into a spirit-soaked dental swab. I watched the patient closely still finding myself surprised to see what such a small dose could achieve. A ‘mask acceptance dose’ they called it in Bristol.
‘I’m just going to put this mask gently onto your face and I want you to breathe quite normally. There that’s fine. Well done. You’re doing very well. Now I’m just going to put this strap on to hold the mask. There that’s all right, isn’t it? Are you comfortable?’
The patient, a woman of 39 years scheduled for hysterectomy, nodded. She breathed the mixture of oxygen and nitrous oxide quietly and easily and I saw the bag on the anaesthetic machine moving in and out as she did so. Two minutes passed. J.C-B leant forward and through a second needle jab injected 15mgs of curare. He waited another minute and then injected a further 30mgs. I thought to myself what an amazing drug was curare. You could lie in a clearing in the Amazonian jungle and shoot a passing parrot with a curare-tipped dart from your blowgun. The parrot would fall to the ground because the curare stopped the nerve impulses crossing to the muscles. It would also stop the muscles of breathing and the parrot would die. Yet you could eat it without coming to any harm, as curare was not absorbed from the gut. Remarkable really when you thought about it.
Suddenly I became aware that something was wrong. The lady had stopped breathing, which was what you would expect, and J.C-B was ventilating her lungs by squeezing the bag on the anaesthetic machine while supporting her jaw and holding the mask closely onto her face. All seemed to be OK with this, yet her colour wasn’t as pink as it should have been.
J.C-B was looking puzzled. He said ‘I think I’ll put the tube down now.’
He quickly picked up a laryngoscope, put it firmly into the patient’s mouth, said loudly ‘give a little cough, Mrs Porter’, and thrust the endotracheal tube down her windpipe. At the same time he turned the nitrous oxide down and the oxygen up to 50%, clearly expecting the patient’s colour to improve. It didn’t. She just got bluer and bluer. What on earth was happening? I could feel the tension building up within the room. J.C-B turned the oxygen right up to 100% but there was no change, except that she looked increasingly ill. I remembered the time in Taunton when I had turned on the wrong high flow switch, so I glanced at the flowmeters, but there was no mistake this time. I felt I should do something so I measured her blood pressure. It was 75/60, and her pulse rate was 90 per minute. I wondered what else I could do to help and began to feel quite desperate when I couldn’t think of anything.
‘I’m not at all sure what is happening,’ said J.C-B, ‘but as she doesn’t seem any better on 100% oxygen than she was on 50% I think we will put her back on some nitrous oxide so that she won’t wake up and become aware of what is going on. I wonder if she has a pulmonary embolus. Let’s see what an ECG shows.’
We connected up the oscilloscope, which showed some depression of the ST segment, but not much else that was helpful.
‘Why don’t we take a sample of arterial blood?’ I suggested. ‘It will show for certain whether the cyanosis is central or peripheral.’ So we took some blood from the femoral artery. To our surprise it was neither pink nor blue, but a rather strange brownish colour that none of us had ever seen before.
‘What on earth can it be?’ I asked. We were all puzzled, and I was glad that I was not carrying the responsibility for what was happening. One of the younger members of the surgical team suggested that it might be chlorophyll from the lymphangiography that had been carried out some days earlier. He said that he had often seen blood of this colour following it. It seemed rather unlikely, but he sounded so positive that for a while he was half believed, and it certainly added to the confusion.
‘Chlorophyll? I have never heard of it being used that way,’ I thought to myself, but presumably they knew what they were talking about, and anyway some explanation was better than no explanation - or was it?
The cardiologist, whom we had asked to come, arrived. He listened closely to the story, and looked at the patient.
‘I don’t think she has had a pulmonary embolus,’ he said after he had examined her, ‘but let’s take her to the lab downstairs and pass a cardiac catheter to see if her right heart pressures are normal. Have you sent some blood off to the lab?’
Yes, they had.
‘Good. Perhaps they can tell us why it looks such a strange colour.’
‘Will you take her downstairs then, John, and I’ll get on with the list,’ said J.C-B.
‘Yes, of course,’ I replied. I asked for an oxygen cylinder and when it arrived I connected the patient to it using equipment that allowed me to ventilate her on the journey to the lift and down to the cardiac catheter laboratory. At the lab I connected her to the anaesthetic machine that was there, giving her 50% nitrous oxide and oxygen so that she would not be aware of what was happening. We lifted her across onto the X-ray table.
‘We should all put on lead aprons before we start to screen,’ said the radiologist. I struggled into one, thinking what heavy uncomfortable things they were.
Soon we were able to look at an image of the patient’s lungs on the X-ray screen. There were several large fluffy opacities scattered throughout the lungfields.
‘That looks like pulmonary oedema,’ said the cardiologist. ‘I wonder what is going on.’ He turned his attention to the task of cutting down onto a vein at the elbow and slipping a catheter into it, pushing it further and further in so that eventually they could see it on the screen as it advanced towards and into the heart.
‘The pressures on this side of the heart are quite normal,’ said the cardiologist. ‘So she hasn’t had a pulmonary embolus. But just look at the lungs. The oedema is getting worse all the time.’
I looked at the screen again. Yes, certainly the fluffiness had spread and some of the patches which ten minutes before had been discrete blobs had expanded to coalesce with other blobs until the lung fields were almost obliterated. My feeling of helplessness was overwhelming. What should I be doing to help this patient?
At that moment a message came over the phone. Apparently something similarly bizarre had happened to the second patient as the anaesthetic was started. So it looked like some kind of poisoning, though from what no one knew. The haematologists thought that the funny colour in the blood was due either to sulphaemoglobin or methaemoglobin, but they were not sure which. Good grief, I thought, I don’t know anything much about those. I knew that one could treat methaemoglobinaenia with a blue drug called methylene blue but I didn’t know the dose and I couldn’t think what could have caused it in the first place. I did not know anything at all about sulphaemoglobinaemia.
‘Perhaps we should we give her some blood,’ someone suggested. ‘It ought to be a good thing to do if she really does have sulphaemoglobinaemia. There are two pints already cross-matched. We could give her those while we take two pints of her own blood off her.’
It seemed a good idea so we set about it, rather messily as it happened, so that by the time we had finished there seemed to be blood everywhere.
The phone rang again. The lab could say for certain that it was methaemoglobin that was giving the blood its brownish colour and that someone was on the way down with some methylene blue.
‘What is the dose?’ I asked.
‘Ten ccs, I think,’ someone said, ‘but I am not really sure.’
‘Let’s look it up then while we are waiting.’
When the methylene blue arrived I looked at it in disbelief. Surely this dark blue fluid in this fragile glass ampoule could not make this poor woman better. Or could it? I drew the dye up into a syringe and slowly injected it into a vein in her arm. At first nothing happened. I continued to watch closely. After twenty seconds I wondered whether there might not be just a tiny change. Within a minute it was unmistakable. The ominous blue colour in the otherwise pale skin was turning pink before their eyes. By the time ninety seconds had passed the transformation was complete.
‘That’s amazing,’ I said. ‘Have you ever seen anything like that before?’
No-one had[1].
The lungs, when I inflated them, were still as stiff as they had been before. This was disappointing because otherwise she looked so much better. She no longer seemed to be about to die from lack of oxygen as she had done just five minutes ago. Perhaps the pulmonary oedema too would get better now, though the X-ray screening of the lung fields showed the fluffiness to be worse than ever.
Someone, I could never afterwards remember who it had been, went upstairs to find out what had happened to the second patient. Apparently when she too became cyanosed as the anaesthetic was started, they had realised that it must be a poisoning of some sort so they had sent for a different anaesthetic machine and had ventilated her with nothing but oxygen from that time onwards. She too had gone pink within ninety seconds of getting a dose of methylene blue and her blood pressure had risen. They had now just reversed the muscle relaxant and had extubated her as well. She seemed to be OK at the moment. They had been trying to work out what was the source of the poisoning. It seemed most likely to be some sort of contamination of the nitrous oxide cylinder, as nitrites were known to cause methaemoglobinaemia. The oxygen cylinder was unlikely to have any contaminant other than nitrogen, which could not have caused the problem, and the manufacturers of the curare had been contacted and said the particular batch of the drug had been in use for some time and there had been no problems reported. The thiopentone was from a multi-dose bottle which had been prepared forty eight hours earlier and no other patients had shown any adverse reaction from its use. There were sending the cylinders back to the British Oxygen Company as rapidly as possible for analysis of its contents. They had abandoned the rest of the operating list.
By this time it was clear that the patient in the X-ray department was not getting any better as far as the stiffness of her lungs was concerned and the whiteout on the X-ray screen was getting worse all the time. We gave her some hydrocortisone to dampen down the inflammation and also a diuretic drug to try to get rid of some of the fluid that was pouring from her lung capillaries into her lung tissues and air sacs, threatening to drown her from within.
Later we moved her to the Intensive Care Unit at the Royal Infirmary two miles away. I ventilated her in the ambulance by squeezing a bag connected to a portable oxygen cylinder just as I had done on the way to the X-ray department earlier in the morning. When we arrived at the ITU there was a Cape ventilator set up ready and waiting for her.
During the afternoon the pressure required to blow the mixture of air and oxygen into her got higher and higher; at the same time the transfer of oxygen across her lungs to her blood became poorer and poorer. Sadly, despite all our efforts, she died during the night.
The second patient, who was fine when she got back to the ward, developed some wheeziness a few hours later, so we moved her to the ITU. as well. Happily she was much improved by the following morning by which time the British Oxygen Company had phoned to say they had found definite contamination of the nitrous oxide cylinder with higher oxides of nitrogen; this was later confirmed as nitric oxide in excess of 1.5%. Though it did not help the one poor lady who had died, it was nevertheless a relief, particularly to the professor, to know that there was a concrete explanation for what had happened.
No-one knew whether there were other cylinders in the city that were contaminated so the use of nitrous oxide was banned until BOC had supplied new cylinders whose purity could be guaranteed. Routine operations were cancelled and only emergency cases accepted for surgery. The younger anaesthetists in the department were completely without experience of any sort of anaesthetic that was not based upon nitrous oxide and relaxants or upon nitrous oxide as a vehicle for other inhalational agents, most usually halothane. Because of this, it fell to the senior registrars and consultants to give the few anaesthetics that were required in the following day and a half before things got back to normal. I could not help thinking how crazy it was that at Southmead Hospital, just four miles away, the juniors were taught the skills of regional anaesthesia, in particular spinals and epidurals. Her at the ‘big’ teaching hospital they actually discouraged their trainees from practising most of the great variety of anaesthetic techniques available, in the honestly held belief that their very limited choice of methods was best for the patients.
Some weeks later, when I thought that discussion about the affair had died down, I was asked by J.C-B. if I could possibly go to Leeds as there was going to be a research seminar there on ‘Higher Oxides of Nitrogen’. They were hoping that someone from Bristol would go along to tell them what had happened on that fateful day. I explained that it was not very convenient really as Isabel and Charlie and I were going to stay with John and Mary in Liverpool for a few days, while Kate and Tim stayed with their granny. But in the end I agreed, rather reluctantly, to travel home on the Friday via Leeds and be there for the afternoon’s meeting. It meant Isabel and Charlie would have to hang around for an hour or two, but never mind
The visit to Liverpool was a great success. John and Mary were excellent hosts and made us feel very welcome. The first evening we met up with Peter and Veronica who were also in Liverpool and enjoyed talking over old times. When Peter had left Catterick he had first gone back to Southmead as a registrar but now he was a senior registrar and actively looking for a consultant post. The following evening the three girls went off to the pictures, while we two Johns baby-sat. The cinema was crowded and they had to sit in the front row of the stalls, which proved a disaster. To watch Omar Sharif at one side of the wide screen when Lara was appearing at the other was rather like being at a tennis match. It quite spoiled the film for Isabel. As there was also an icy draught round her feet she said that she felt as though she was in Siberia anyway.
Leeds was in bright sunshine when we arrived just before one o’clock on the Friday. We motored around till we found Hyde Terrace where the anaesthetic department was housed. This proved to be some distance from the hospital, which seemed odd. We ate the sandwiches that we had brought with us and then I went into the building and introduced myself to the secretary. The meeting was about to start.
There were twelve or so people in the room including Dick whom I had known at Catterick. There were others who, unknown to me at the time, were later in life to become either temporary or permanent colleagues of mine in Bristol - namely Godfrey, Ronnie, and (last, but not least) Cedric. I was very nervous and I was considerably overawed both by the occasion and by the eminence of the professor who was on loan to Leeds University from the Medical Research Council while the hospital and Clinical Research Centre at Northwick Park was being built. I stumbled through the story I had to tell, concentrating mainly on the clinical details. There were a few questions asked and I answered as best I could. I then excused myself explaining that I had a wife and child in a car outside and we were actually on a journey from Liverpool to Bristol.
I forgot all about the meeting until the following May when the British Journal of Anaesthesia devoted a whole issue to discussing Higher Oxides of Nitrogen as an Impurity in Nitrous Oxide. There was an graphically written account[2] by J.C-B of the events of that terrible day in September 1965, and amongst other articles, historical and chemical, there were reports of the results of the various research projects that were being planned the very afternoon that I had visited Leeds. Clearly the department there was highly professional and most effective in its approach to research for it was remarkable to have planned and completed the different studies in such a short time. It seemed quite a contrast to the splendidly eccentric and slightly amateur approach to research that was favoured in Bristol. Still I could not deny that it was very relaxed and comfortable in the city where Humphry Davy had first experimented with nitrous oxide, and where he had written in 1800[3]:
A considerable time elapsed before I was able to produce the gas in a state of purity, and my first experiments were made on the mixtures of nitrous oxide, nitrogene and Nitrous gas (Nitric oxide)....
So 1965 had not been the first year that someone in Bristol had breathed nitrous oxide contaminated with nitric oxide. It was lucky that Davy had not done himself a serious injury!
Denver, Colorado
‘The air is a bit thin here in Denver for that sort of anaesthesia, John,’ said Bob. ‘Why, the atmospheric pressure is only 628 millimetres of mercury and not the big 760 that you are used to. It means that 70% nitrous oxide sure is a lot less powerful than at sea level.’
I had been describing once again the type of anaesthesia that was used so routinely in Bristol, but this time too I failed to raise any enthusiasm in the ‘Mile High City’ for the unsupplemented nitrous oxide-relaxant technique. I realised that I was in danger of becoming a bit of a bore because of the way I went on about it, but still I couldn’t stop myself.
Dave, who had been scribbling on a piece of paper, looked up and said ‘I’ve just worked out that 70% nitrous oxide in Denver is roughly equivalent to 57% at sea level if you allow for water vapour.’
‘But we often use less than 70% nitrous oxide,’ Ted chipped in from the back of the room. ‘You know we often give more oxygen in Denver because of the altitude, so we may not have 70% nitrous oxide to start with. If we use 60% here it’s only equivalent to 49% at sea level. You wouldn’t be happy with that now, would you, John?’
‘Not really,’ I admitted reluctantly. ‘Though I expect it would be all right if you hyperventilated the patients like they do in Liverpool. It does seem to deepen the anaesthesia in some way or other, possibly due to the change in pH.’
‘Perhaps we should try it out some day,’ said Ted. ‘We could sample arterial blood at the same time and check the oxygen tension. It’s time we did that anyway at altitude now that oxygen electrodes are both available and reliable.’
‘Why, that’s true enough,’ said Bob. ‘Perhaps you and John could get the electrode working and plan a small study.’
It took us several weeks to get the electrode working to the accuracy we needed, but eventually it was time to start the study. We decided that it would be all right to use 70% nitrous oxide - 30% oxygen for the anaesthetic, since we would be measuring the level of oxygen in the patient’s blood throughout the operation and we would know whether it was O.K. or not. If it was low we would be able to increase the inspired oxygen concentration easily enough. Ted became expert at putting a needle into the radial artery, and I at changing the membrane on the tip of the electrode.
We studied fourteen patients altogether. One of them said afterwards that she had had a peculiar dream and she wondered if she had been properly asleep during the operation, but, no, she hadn’t felt any pain. She remembered her blood pressure being taken and had been aware of people moving about the room and of voices, though she didn’t recall what was said. It puzzled her rather than bothered her.
The oxygen levels in the blood samples were mostly satisfactory, but in three patients they were rather low at times, though not dangerously so. At the end of the study when we wrote it up we felt that we had to recommend adding extra anaesthetic to the nitrous oxide and giving at least 40% oxygen if the levels of blood oxygenation were not being monitored. It was fortunate that the misprint in the paper when it was published in the ‘Yellow Peril’ (Current Researches in Anesthesia and Analgesia) was not of any clinical importance, but it irritated me all the same. The typesetter obviously had made the mistake, but the proof-reader, me, should have spotted it.
They would have printed my photograph at the beginning of the article had I not forgotten to send it to them.
Southmead Hospital, Bristol
Humphrey and I both started at Southmead on April Fool’s Day. It would have possible for me to begin a month earlier, but it had seemed wrong somehow to get there before the surgeon with whom I was going to work, so I delayed my own arrival.
Once I did get there I found things very different from the Infirmary. Not only was regional anaesthesia practised and encouraged, in particular epidurals, but tiny doses of thiopentone and the unsupplemented nitrous oxide-oxygen-relaxant technique were scorned. Of course, I was already used to adding a volatile agent to the nitrous oxide from my times in Taunton and Catterick and Denver. Nevertheless it was a great relief to me to no longer feel that somehow I was letting the side down if I did turn on the halothane or give an intravenous opiate, or even both. At least you could be sure that your patient would stay asleep if the nitrous oxide ran out, and so the risk of awareness under anaesthesia no longer existed.
There was talk of new theatres being built at Southmead. There was also to be a Central Sterile Supply Department so that instruments would not need to be sterilised in the theatre suite itself. It would be pleasant not to have to put up with the high humidity produced by the steam sterilisers, which at the moment caused the theatre walls to drip with water unless you opened the windows. Still the moisture in the air did keep the static electricity down and made explosions unlikely when ether and cyclopropane were being used (see chapters 3 and 4).
The new theatres were almost ready for use, but first the gas outlets needed to be tested. I borrowed the Hudson oxygen analyser from the Intensive Care Unit, and the engineer, the pharmacist and I went around testing the various outlets. Really it was quite simple: the suction should suck; the air was not yet connected; oxygen should read 100% and nitrous oxide 0%. In the event it was surprising how much we had to flush the pipelines to get the figures even to approach the extremes.
‘Of course,’ I said, ‘as we are only looking at two different gas supplies here, we can identify the outlets and confirm that the connections are OK even before the flushing is complete.’
‘That may be true but I am not signing anything till we get the air out of the pipes.’
He was quite right, of course. After all there had been a tragedy in Edinburgh when nitrous oxide had been connected to the oxygen lines[1], and some sick patients on a ward had been given nitrous oxide instead of oxygen. We certainly did not want to make any mistakes.
‘Its a pity we haven’t got a whistle; that would tell us which gas we had in the pipeline.’
‘A whistle? How would that help?’
So I told them about J.C-B’s organ pipes.
‘Perhaps one day we should explore the notion of a whistle that you just plug in to the outlet identify the gas by the note it produces.’
‘It sounds a splendid idea.’
We never did get around to it.
‘I am sure we don’t use the closed circuit often enough,’ I said to my young colleague. ‘It really does have many advantages, you know. For a start it saves a lot of gas and the patient gets something warm and wet to breathe, instead of this cold dry stuff.’ I pointed vaguely in the direction of the anaesthetic machine. ‘In many parts of the world they use it all the time. I think in Britain in the fifties and sixties we often used such light anaesthesia with our relaxants that it became important to know for certain that the concentration of nitrous oxide could not fall, or the patient might wake up. So we used high gas flows to keep the anaesthetist relaxed as well as the patient. It fitted in well with ‘minute volume divider’ ventilators, and in addition we were using a lot of Trilene in those days. Trilene, of course, isn’t compatible with the soda lime in the carbon dioxide absorber.’
‘Presumably you have to offset the cost of the soda-lime against any savings you make by using less gas.’
‘Yes, of course, you do, but soda-lime is relatively cheap and the economics are heavily in favour of circles with low flows. Just look: at the moment we are using five litres a minute of nitrous oxide. How many litres is that in two hours?’
‘Let’s see. Five times sixty times two equals... six hundred.’
‘And how many litres do you think there are dissolved inside a patient after two hours anaesthesia?’
‘I haven’t any idea. How many are there?’
‘Well, let’s work it out. Years ago Severinghaus produced an equation that approximated to the uptake of nitrous oxide in some patients that he had studied[1]; the rate, in millilitres per minute, was one thousand divided by the square root of time, in minutes, from starting to breathe the stuff. I’ll write that down.’
I wrote:
uptake of N20 (ml/min) = 1000 /
(min)
‘Of course,’ I continued, ‘Severinghaus used the proper scientific notation and wrote it as 1000t -0.5 but I always find that too bizarre a mathematical concept to be credible. Now let’s take an anaesthetic chart and we’ll use the blood pressure grid as a piece of graph paper to plot some points of uptake against time for two hours. Then we’ll draw a line and count the squares underneath. That way we’ll know how much nitrous oxide is absorbed.’
After a false start and a few minutes the graph was completed. With the eye of faith we counted forty two squares beneath the line, or was it forty three?
‘How much is each square worth?’
‘Well, each square is 100 ml/min for five minutes; that’s half a litre. So forty two squares, or thereabouts, is twenty one litres. It means that after two hours your patient has only got twenty litres or so of nitrous oxide inside him even though you have used six hundred litres. That seems pretty wasteful, doesn’t it?’
‘I see what you mean. What does six hundred litres of nitrous oxide cost?’
‘I don’t know, but it is one third of the contents of the spare cylinder on the back of the machine. Perhaps you could find out for me sometime.’
‘Yes, certainly I will.’
‘Of course, twenty litres is also the amount of nitrous oxide that has to come out of the patient at the end of the operation. It’s what causes the diffusion hypoxia we were talking about earlier, especially if there is any respiratory depression and we don’t give the patient added oxygen to breathe for the first five or ten minutes. Let’s see now, twenty litres is about the same volume as five gallons of petrol.’
‘Or forty pints of beer!’
‘John,’ said Mike, ‘you’re just the man to answer the question one of the students asked me this morning.’
‘It is always a mixed blessing to be challenged like that,’ I replied. ‘If you can come up with the answer it is quite gratifying; if you can’t you feel a complete failure.’
He laughed.
‘So what was the question?’
‘If a cylinder of nitrous oxide is full of liquid, why can’t you hear a splash when you shake it?’
It was my turn to laugh.
‘I was not expecting anything like that,’ I said.
‘Nor was I.’
‘I should think it is just a matter of viscosity. After all you wouldn’t hear a splash if you shook a tin of treacle, would you?’
‘That’s what I thought. I just wondered if I was right.’
‘I should think so. After all gaseous nitrous oxide is two and a half times heavy than air; liquid nitrous must be many times heavier again. There’s 1800 litres of gas squashed into that cylinder, you know. Why don’t you look up the viscosity of liquid nitrous oxide and let me know.’
‘I’ll do that, John,’ he said.
I am still waiting to hear what it is[1].
Thirlmere, The Lake District
The cottage at the south end of Thirlmere was splendid. As Isabel wrote in her journal:
Saturday, September 26th. ........it nestles in a lovely valley, with views of craggy hills and a sparkling burn. There are sheep grazing directly outside the sitting room window which slides open, so that it is like sitting in the field with them. Immediately opposite was Nabs Crag, which is part of Wythburn Fells, and Helvellyn towered above us away to the east.
After supper I glanced through the guidebook.
‘Isabel, it says here[1] that Humphry Davy climbed Helvellyn in 1805, with William Wordsworth and Walter Scott. And they set out from Wythburn church. That’s less than half a mile from here.’
‘You can put any idea of us climbing Helvellyn right out of your mind,’ she replied. ‘We are not fit enough for anything like that.’
‘Well, Walter Scott climbed it, and he had a withered leg from polio as a child[2].’
‘That’s as may be, but he was a lot younger and fitter than we are. If we ever do get around to climbing it, it’ll only be if we set out really early one morning, so that we have plenty of time.’
She told me later than she knew with a frightening clarity that we would be climbing it before our two weeks were up.
We spent the next day up climbing to Greenup Edge, and we were both encouraged by how well we felt after our exercise, though we were very tired, and in dire need of a gin and tonic.
By the following Thursday evening we had, to both our surprise, climbed Skiddaw, which at 3,054 ft was only 62 ft less than Helvellyn. I smiled quietly to myself; we would get up Helvellyn after all! It was a point of honour, was it not, for anaesthetist to follow in the steps of Humphry Davy?
I will let Isabel’s journal tell the story of that day:
Tuesday 6th October. Wythburn church carpark to Helvellyn, and back: I had said that I would only contemplate this climb if we could be on the fell by 8.30 am. at the latest. Consequently when I awoke at 3.30 am. to find John no longer beside me, I knew what he was doing - making sandwiches. He did not admit this till later in the day, but my surmise was correct.
We set off at about 8.30 am. through a pine forest with an unremitting upward slope. I had to go into fifty paces mode almost at once. For a little while there was a fence on my left which helped to haul me up the slope, but that soon petered out and I was left to my own devices. Attempts to form a firm path also petered out quickly to be replaced by an ankle turning jumble of rocks and stone of various sizes that boded ill for the descent.
The relative shelter of the wood and the curvature of the early slopes left us quite unprepared for the screaming wind which attacked us just as we reached the steepest part of the climb. By this time the summit had disappeared and lowering above us in all directions was a thick mist. The mist descended very low and the wind increased in intensity.
(I really thought for one moment that we were going to be plucked off the side of the mountain by the wind.)
We felt very lonely and both a bit scared. It was now also raining very hard and was cold. Reluctantly John decided that this wasn’t the day and that we should turn back - I say John decided, because I was so scared I would have turned back half an hour before we did!
We had just begun our descent when leaping up the path came two men, who asked what it was like at the top. John explained we were turning back and I said it was because I was scared. The older of the two men said ‘ Nonsense, coom oop wi’ us. It’d be smashing if we could get you t’top. You’ve doon the wurst, and it gits flat in a minute.’ Irrestible! John was scampering off upwards. I had to abandon my fifty paces mode, and shoot up the fell until I thought my heart would burst - I am sure it nearly did! It was always ‘going to be flat in ten minutes’, and of course I couldn’t shout or swear at him.
All this time the wind was screaming in our faces and the rain stinging our cheeks. Eventually when they got us of the flattish! path they went on ahead to the summit, saying that it was only about another two hundred feet. I, of course, thought they meant along, but actually they meant upwards. However we floundered along in the mist groping our way from one cairn to another, without being able to see anything at all. We met the men on their way down. Still encouraging, but warning us to return immediately we arrived., as the mist was even thicker on top, the path flattened out and there might be no land marks to help us pick it up again. This did a whole lot for my confidence, but nothing daunted we struck off again. At the top there was a sort of a shelter into which we stumbled. It wasn’t a shelter really, more like a wall built against the prevailing wind with a sitting ledge. It was wet and FREEZING. The shelter was already occupied by a lone fell walker, clearly of the intrepid variety, complete with knee-length trousers, long red socks, red hat etc., who was studying a map and compass, trying to descend by a different route to complete the round, having just come up via Patterdale and Striding Edge.
It was with amazement that both he and I looked at John taking out a lunchbox from his rucksack and heard him offer me a hard-boiled egg. The offer was accompanied by regret that he couldn’t take the shell off as his hands were numb with cold. I did not laugh at the time...
( She certainly did not! But I swear I heard her say ‘bugger Humphry Davy’.)
... not a muscle in my face twitched, but I have since become helpless with laughter each time I think of the incident. The hard-boiled egg was followed by cheese sandwiches. Soon our acquaintance got up to leave. He had decided to descend via High Park Wood. We said our good-byes and set about getting ready to leave when an amazing thing happened The wind did not abate, but the rain stopped and the mist seemed to boil and swirl all around us. We looked over the parapet of the shelter wall and there spread out before us was Ullswater, Swirral Edge, Striding Edge and all the rest of the Lakeland fells tailing off into flat land as far as the eye could see.
(Less than a minute earlier I had looked up at the sky and said ‘come on, God; if you really are up there, give us a sign’. I don’t know if this had anything to do with it or not.)
The wind was bitterly cold, and perhaps made worse because our clothes were so wet. It was truly awesome. After a while we could stand the cold no longer, even though we had wrapped some spare socks around our frozen fingers, and we began descending.
This was now another world from the one in which we had journeyed upwards. Spread out were all the views we had missed: from the far left the Solway and Windermere, taking in Wythburn valley, Greenup Edge, Middle How, Ullscarf High Seat to Derwentwater. Backing the ‘front range’ we could see Langdale Pikes, Great Gable and the fells surrounding Wasdale, the Old Man of Coniston, and the fells behind Derwentwater to Skiddaw on the far left. What a gift. It was quite unforgettable. The whole thing was set off by the entire length of Thirlmere in the fore ground. It was like a mammoth geography lesson, and we were able to trace out some of the walks we had made and the features we had seen upon them like Harrop Tarn.
Part way down we slept in the sun in the lea of a friendly rock for some time, and then watched the rest of the world toiling up to the summit, bathed in a glow of self-satisfaction, though we would never have had it if it hadn’t been for those two men, who were long gone by now.
I will draw a veil over the rest of the descent as it was awful, and I was wimpy due to crumbly knees. However, it was an experience that I wouldn’t have missed, and the memories will be there forever.
After supper that evening we drank a toast to Humphry Davy and nitrous oxide. Isabel said she knew now what it must have been like for Sir Walter Scott with his gammy leg, and that it was a pity that they didn’t give you laughing gas half-way up Helvellyn!
It is now 148 years since Horace Wells had his tooth pulled under the influence of nitrous oxide, and a third of a century since I took up anaesthesia as a career. Though we know to-day that nitrous oxide is more reactive in the body than we had previously thought, my colleagues and I at Southmead still use it in the great majority of general anaesthetics that we give. I personally limit the concentration to 50%, so that if bowel distension does play any part in causing postoperative nausea, I cannot more than double the bowel gas content even in the longest operations. However things are certainly changing in some other centres; Cedric tells me that he has given up using nitrous oxide altogether.
‘It doesn’t really add much to a modern anaesthetic, you know, and I’m sure that it causes nausea. In the States they call it "the English gas".’
Cedric is into total intravenous anaesthesia in a big way, of course.
‘What about gas inductions in children? They are still occasionally necessary, and we don’t have cyclo around to help us any more.’ [see chapter 4]
‘Yes, that’s been the only slightly awkward thing about not using nitrous oxide, but with a little practice you can manage with ethrane on its own, using oxygen-air as a carrier gas rather than oxygen-nitrous oxide.’
I expect he is right. I wonder if any of us will be using nitrous oxide in twenty years time.
Incidentally, the background level of nitrous oxide in the air has risen by more than 7.5% since 1940[1] or thereabouts. This is probably a result of the increased use of nitrate fertilizers throughout the world.
I calculate that at my present weight (or should it be volume?) there are of the order of half a British trillion (500,000,000,000,000,000) molecules of nitrous oxide within me as I write this line - and, of course, within you, too, as you read it.
NOTES
[1] calculated from Loschmidt’s constant (2.69 x 1019 ), which is the number of molecules in 1 cm3 of an ideal gas at NTP; the following assumptions were made: nitrous oxide concentration in air in 1933 = 287 ppbv [3], diameter of ovum = 150 microns, blood/ovum partition coefficient = 1.0 and body temperature =37oC.
[2] laughter from inhaling nitrous oxide was first recorded by Humphry Davy in 1799, some 45 years before it was used as an anaesthetic. Of his experiments at the Pneumatic Institute in Bristol in April and May 1799 he wrote:
Generally when I breathed from six to seven quarts, muscular motions were produced to a certain extent; sometimes I manifested my pleasure by stamping or laughing only; at other times, by dancing and vociferating.
Davy did not refer to nitrous oxide as ‘laughing gas’ in his thesis[4] , though he reported laughter occurring in many subjects, including Samuel Coleridge, the poet, in addition to himself.
[3] Khalil M. and Rasmussen . Nitrous oxide: trends and global mass balance over the last three thousand years. Annals Glaciol. (1988) 10: 73-79.
[4] Davy H. Researches, chemical and philosophical; chiefly concerning nitrous oxide. London: Johnson J., 1800.
[1] My mother recalls that she had ‘gas’ during each of her labours. She probably received gas-and-oxygen from an intermittent flow machine such as the McKesson, of which there was a small compact obstetric model. Langton Hewer, in Recent Advances in Anaesthesia and Anaesthesia, 1932 (J & A Churchill, London) recommended:
As soon as the pains become severe the mixture control is set to 10% oxygen, 90% nitrous oxide, the facepiece is placed in position and the patient instructed to take three deep breaths, holding the third one at the end of inspiration and at the same time ‘bearing down’.
Although Minnitt presented a paper[a] on his gas-and-air machine to the Royal Society of Medicine on 4th May 1934, this was only six weeks before I was born, and the apparatus is not likely to have been found at the relevant moment in a small nursing home in Carlton Drive, Putney. There remains the possibility that my father brought along the McKesson machine from his dental surgery. I have a vague memory of discussing this with him once, but I cannot be sure that I am not indulging in fantasy here. In any event the calibration of early models of on-demand gas and oxygen machines, such as the McKesson, was highly suspect. In a study[b] of five machines of standard design, regularly serviced and in regular use, it was found that with the control setting at 10% the actual concentrations delivered varied between 1.7% and 20.1%.
[a] Minnitt RJ. (1934) Self-administered Analgesia for the Midwifery of General Practice. Proc. Roy. Soc. Med. 27: 1313. [b] Bourne J. (1960) Nitrous Oxide in Dentistry - Its Dangers and Alternatives. London: Lloyd-Luke [Medical Books] Ltd.
[2] When a pregnant woman inhales nitrous oxide the concentration rises more slowly in the foetal tissues than in her own. This is because there are two points in the transfer where blood with high concentration of nitrous oxide comes into contact with blood of low concentration, first the placenta and then the foetal heart and great vessels. It has been calculated that with nitrous oxide it would take 40 minutes before foetal and maternal tissues were in near-equilibrium[c]. Also, nitrous oxide is only inhaled intermittently during labour and then mainly while the uterus is contracting and the blood flow reduced. My exposure in utero may have been considerably less than I originally thought.
[c] Dawes GS. (1973) The distribution and actions of drugs on the foetus in utero. Brit. J. Anaesth. 45: Suppl, 766.
[1a] It isn't! The 'Nelson houses' on the north side of the Upper Richmond Rd west of Quill Bridge were built c. 1865 and named after the sister of the third Earl Nelson - see Putney and Roehampton Past ed. Dorian Gerhold 1994, reprinted in 2000 by Historical Publications Ltd.
[1] there was little public awareness of the dangers of asbestos until the 1970s, though Pliny[a] wrote in 50 BC of respirators used to prevent dust being inhaled by weavers of asbestos.
[2] laughing occurs during what Harris[b] called the happy inebriation of the co-operative stupor stage of depression of the higher centres of the brain. This corresponds to lower stage I of the Guedel classification[c] . The stages of anaesthesia are discussed in more detail in later chapters, especially chapter 11, 1954.
[a] quoted by Hunter D. in The Diseases of Occupations 6th ed. London: Stoddart & Houghton, 1978; p 990. [b] Harris TAB. The mode of action of anaesthetics. Edinburgh: E & S Livingstone, 1951. [c] Guedel AE. Inhalation Anesthesia. New York: The Macmillan Co., 1937.
[1] Five years earlier Waters[a], in a survey of 10,638 anaesthetics, found that vomiting occurred in 23% of patients who had had nitrous oxide (cf. ethylene: 33%, cyclopropane: 39%, ether: 56.5%). However, in this era nitrous oxide was commonly given with less than 20% oxygen, and anoxia is known to be a potent cause of nausea. This incidence is, therefore, not relevant to modern anaesthetic practice. [a] Waters M. (1936) Brit. Med. J.; 2, 1013.
[1] The ability of nitrous oxide to admit a candle to burn in it was discovered by Joseph Priestley[2] in 1772 during his original work isolating and recognising the gas, which he called dephlogisticated nitrous air; Humphry Davy[3] confirmed the observation 27 years later.
[2] Priestley J. Experiments and observations on different kinds of air. 2nd ed. London: J. Johnson, 1776.
[3] Davy H. Researches, chemical and philosophical; chiefly concerning nitrous oxide. London: Johnson J., 1800.
[1] Harris T.A.B. The Mode of Action of Anaesthetics. London: E & S Lingstone Ltd, 1951.
[2] Davy H. Researches Chemical and Philosophical, chiefly concerning Nitrous Oxide. London: J. Johnson, 1800.
[4] Macintosh R., Pratt Freda B. Essentials of General Anaesthesia, with special reference to dentistry. Oxford: Blackwell Scientific Publications Ltd, 1940.
[5] In 1957 Langton Hewer and Lee’s Recent Advances in Anaesthesia and Analgesia [London: J & A Churchill Ltd, 1957] still recognised the use of reduced oxygen:
On the other hand, when it is used as a sole anaesthetic in robust patients, its weak properties demand that it should be combined with less than 20% oxygen in order to secure the patient....
Secure the patient? That was some way to describe it! However, this sentence was followed by a caveat:
In these circumstances, the associated hypoxia may, on occasions, cause serious complications and irreversible neurological changes. What cannot be cured had better be prevented.
In the next edition of Recent Advances, which was published in 1963, Parkhouse recognised that much of the dental anaesthesia in the country still consisted of nitrous oxide with reduced oxygen, but he stated firmly that:
...it should be unnecessary, at the present time, to use anoxia as an adjunct to anaesthesia.
I am sure that it was the increasing use of halothane (see chapter 6) that finally got rid of the old hypoxic techniques in dental anaesthesia.
[1] My friend Jim Sheeran would be disappointed if I did not recall that the word ‘trachea’ means ‘rough’ (artery) and comes from the Greek t r a ch e a (a r t e r i a ).
[2] High flow levers for nitrous oxide were there to help at the induction of anaesthesia using 100% nitrous oxide. In contrast, modern machines are designed so that hypoxic mixtures of nitrous oxide and oxygen cannot be given under any circumstances.
[1] Clutton-Brock J. (1961) Pain and the barbiturates. Anaesthesia 16:80
[2] Clutton-Brock J. (1957) The cerebral effects of overventilation. Brit J Anaesth. 29:111
[3] a ‘grain’ is the smallest of the old British weights and is the average weight of a seed, or grain, taken from the middle of an ear of corn. It is about 1/7000 of a lb avoirdupois, or 60mg. This explains why many drugs are marketed to-day in doses that seem unlikely in metric terms, e.g. ephedrine 30mg (gr 1/2); atropine 0.6 mg (gr 1/100); hyoscine 0.4mg (gr 1/150); aspirin 300mg (gr v). Sadly the use of British weights in pharmacy was discontinued in the 1970s.
[4] in later years I was to think that the margin for error with this technique was too fine to be acceptable. The risk of ‘awareness’ during anaesthesia, even if only of the spoken voice, was not worth taking merely to avoid a slightly deeper level of anaesthesia.
[1] Cole P. Nitrous oxide and oxygen from a single cylinder. Anaesthesia. 1964; 19:3
[2] Tunstall M.E. Effect of cooling on pre-mixed gas mixtures for obstetric analgesia. Brit. Med. J. 1963; 2:915
[3] I was sure it was Andrew, but he denies it. I wonder who it was. If it was you, do drop me a line.
[4] Although Davy wrote of nitrous oxide as the pleasure-producing gas[a], not all his subjects found it pleasant;. in particular, Joseph Priestley, who had prepared and isolated the gas in the first instance in 1770,
..generally had unpleasant fullness of the head and throbbing of the arteries, which prevented him from continuing the respiration.
So at least I can console myself that I am in good company!
[a] Davy H. Researches Chemical and Philosophical, chiefly concerning Nitrous Oxide. London: Johnson J. 1800.
[1] Eger E.I, II, and Saidman L.J. Hazards of nitrous oxide anesthesia in bowel obstruction and pneumothorax. Anesthesiology, 1965; 26: 61.
[2] Eger E.I, II, and Saidman L.J. Change in cerebrospinal fluid pressure during pneumoencephalography under nitrous oxide anesthesia. Anesthesiology, 1965; 26: 67.
[1] Years later I came to enjoy asking the riddle ‘when does blue + blue = pink’. It was only rarely that anybody guessed the answer.
[2] Cutton-Brock J. Two cases of poisoning by contamination of nitrous oxide with higher oxides of nitrogen during anaesthesia. Brit. J. Anaesth. 1966; 39:8
[3] Davy H. Researches Chemical and Philosophical, chiefly concerning Nitrous Oxide. London: Johnson J. 1800.
[1] Editorial. (1966) An accident in Edinburgh. Lancet. Oct.29th.
[1] Severinghaus J. The rate of uptake of nitrous oxide in man. J. Clin. Invest. 1956; 1813.
1986
[1] On January the 23rd 2006 I received the following e-mail from an old friend:
Hello Sir!
I refer to your website page relating to nitrous oxide, 1986, and the question of lack of splash when shaking a cylinder of the stuff. Today I carried out an experiment! A size E cylinder was balanced horizontally on a laryngoscope handle to resemble a see-saw made from a plank on a log. The cylinder was see sawed just a few degrees gently up and down by hand so that the cylinder was not allowed to touch the ground, but was always being held at the end. At the end of each stroke, with a delay of about half to one second, it was very easy to sense a slight jolt as the liquid splashed down to the lower end of the cylinder. Therefore the liquid appears to flow in a manner similar to a watery substance. Certainly it is not at all like engine oil, or treacle. I would estimate that its viscosity is in the same order of magnitude as water!
With very best wishes, Ian Norley.
I replied: What a splendid experiment! I am sure you are right. I have just spent a few minutes surfing the net and have discovered the density of liquid nitrous oxide is 1.22 compared to water, so the viscosity is, as you say, probably similar too. I have emailed BOC to see if they can tell us, but I bet it has never been measured by anybody anywhere. Which still leaves us wondering why you can't hear any splashing if you shake it. Perhaps your next experiment should be to fix a stethoscope to a cylinder and see if you can hear a splash that way. It may just be the thickness of the metal that that stops the sound.
He duly tried this out but still 'didn't hear any sloshing'. I never heard from BOC.
[1] The Ordnance Survey Landranger Guidebook to The Lake District. 1st edition. Southampton: O/S, & Norwich: Jarrold, 1988, page 59.
[2] Though poliomyelitis was not described in the medical literature until 1789[a], Walter Scott, who was born in 1771, was the earliest case on record in the British Isles[b]:
I showed every sign of health and strength until I was about 18 months old. One night, I have often been told, I showed great reluctance to be caught and put to bed, and after being chased about the room, was apprehended and consigned with some difficulty. It was the last time I was to show much personal agility. In the morning I was discovered to be affected with the fever which often accompanies the cutting of large teeth. It held me for three days. On the fourth when they went to bathe me as usual, they discovered I had lost the use of my right leg.
[a] Underwood M. A treatise on the diseases of children with general directions on the management of infants from birth. 2nd edition. London: Matthews, 1789.
[b] Lochkhardt’s Memoirs of the Life of Sir Walter Scott, Bart, 1837.
[1] Khalil M. and Rasmussen R. Increase and seasonal cycles of nitrous oxide in the earth’s atmosphere. Tellus 35B, 1983: 161-169.
email mailto:johnpowell.net