Sunday
Eddie phoned at four in the morning.
‘Hello,
John. Sorry to wake you at this unearthly hour but we need your help.
We’ve got a lady here who is booked for elective section at the end of
the week but she has gone into labour early. When she came in late
last night I thought she would last till morning but she won’t.’
‘When did
she last eat?’
‘Not since
six last night. That’s ten hours ago now.’
Good, I
thought, I won’t have to empty her stomach.
‘I’m on my
way, Eddie. Could you give her some atropine, please?’
When I got
there I mixed up some Pentothal and got the Scoline from the fridge
while the midwife fetched the patient.
‘Hello, Mrs
Evans, I’m just going to give you a little injection and you will soon
be off to sleep.’
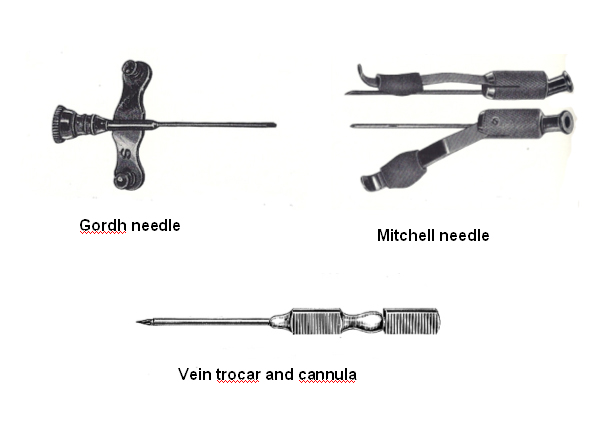
I chose a
vein on her forearm and slipped a Gordh
needle into it. I
injected the Pentothal. I waited for a few moments till she became
unconscious and then quickly injected the Scoline. Just as I finished
doing this the lady half sat up and began to vomit copiously. There
were pints and pints of the stuff. I watched with horror as it
trickled down her chin and out of her nostrils. She retched again.
Clearly I had not given her enough Pentothal and she was still light
enough to vomit actively so she was probably still able to shut her
larynx, thank heavens. I thought about the relaxant drug that was even
now on its way round the circulation. When it arrived at the muscles
and they twitched and lost their power to contract she would be
defenceless against the vomit still in her mouth. She would not be
able to keep her larynx shut and there would be nothing to stop it
going down her windpipe. What should I do?
But there
wasn’t time to think.
‘Hold on to
her legs,’ I shouted at the midwife who was there to help me, and I
tipped the top half of the patient’s body over the side of the trolley
so that her head and shoulders were hanging upside down . The fluid
that she had vomited drained out of her mouth and nose. I clapped the
anaesthetic mask onto her face and pressed the emergency oxygen button
so that the bag filled with oxygen. I squeezed the bag vigorously and,
as the vomit drained downwards into the mask and the tubing which led
from the anaesthetic machine, the oxygen bubbled upwards through the
vomit and filled her lungs. To my relief she remained a wonderful pink
colour throughout.
When the
Scoline had worked and I had sucked out her mouth and throat with the
sucker we lifted her back properly onto the trolley and I thrust an
endotracheal tube down her trachea. The moment of crisis had passed.
The operation was otherwise uneventful and mother and baby did
splendidly. It was many a year before I anaesthetised a woman in
labour without first putting down a stomach tube.
The
night-time emergency work was unrelenting. It was particularly bad
when Arthur went away for two months, and I found myself the only
member of the junior anaesthetic staff. I was first on call for
emergencies every day and night, except that every third weekend I was
off call from Saturday lunchtime to Monday morning.
‘Not
another ‘perf’?!’ I said one night to Henry, the surgical registrar.
There seemed to be more perforated duodenal ulcers than ever this
year. Certainly there had been more ‘perfs’ than appendicitis in the
last month.
‘Has he got
a Ryle’s tube down?’ I asked.
‘Yes, the GP
put one down while he was waiting for the ambulance.’
‘Good. Send
him up and we’ll get on with it.’
It not take
Henry long to sort out a perforated duodenal ulcer - a quick midline
incision, a suck round the peritoneal cavity, to get rid of any fluid
that had leaked, find the ulcer, oversew it and stick a piece of
omentum over the top, cobble the incision together, and there you
were. All done in twelve minutes.
It was now
three in the morning, but I still could not go home for Eddie was on
the phone.
‘John, I
have a young lass here, a primip, who needs the forceps put on. Could
you come across as soon as possible.’
‘I’m on my
way.’
All but the
easiest of forceps deliveries were done under general anaesthesia,
which kept me busy even when the general surgeons were quiet. I
finally got home at six in the morning. I was so tired that I found
myself crying with exhaustion.
‘I’ve been
asked to start one of the lists as the consultant is going to be
late.’
Isabel put
her arms around me.
‘You cannot
go on like this, John. You’ve been on call for the last seven nights
and they still want you to start and finish their lists for them. It
won’t do, you know. Sit down quietly and I’ll make you a cup of
coffee; then you can go off to bed.’
She got up
and left the room for a few minutes. When she came back she gave me
the coffee.
‘Just
swallow this, darling. It may taste a bit funny but I want you to
swallow it all the same, there’s a good lad.’
Hardly aware
of what I was doing I swallowed the coffee even though it tasted
horribly bitter.
‘Now off to
bed,’ she said firmly. ‘Don’t you worry about starting anybody’s list,
John. I’ll phone Dr Gavin and tell him that you are not coming in till
you are feeling better. They will just have to manage somehow without
you.’
I was soon
tucked up in bed and fast asleep. I did not know that she had opened
two yellow Nembutal capsules and had poured the white powder into my
coffee. No wonder it had tasted bitter despite the huge amount of
sugar she had put into it.
When she was
sure I was properly settled Isabel phoned the consultant in charge.
‘Good
morning. It’s Isabel here. I’m phoning to tell you that John arrived
home at about six this morning and he was so exhausted that he was in
tears. I have given him three grains of Nembutal and he won’t be
coming back till I think he is fit to do so. I really don’t know what
you are all doing allowing him to be up night after night. And on top
of that you expect him to start your theatre lists for you, and finish
them too. I think you should all be ashamed of yourselves!’
For a moment
there was silence; then
‘I’m sorry,
Isabel, if we have been overworking him. Of course he must have a
proper rest if he is that tired. I did not realise we were working him
so hard.’
‘Well, if
you and the other consultants didn’t realise, who on earth did you
think would notice something like that? I’ll phone you to-morrow to
tell you whether he will be back on Thursday or not.’
She put the
phone down.
When she did
let me go back to work after two days I was told that in addition to
my having every third weekend off from Saturday lunchtime to Monday
morning I was also to have eight hours off every Friday afternoon
(from 2 pm to 10 pm) - though I would have to come back to cover the
night, of course. They said also that they were trying hard to get a
replacement for the missing registrar so that I would then only have
to do alternate nights instead of every night. Still, they said, with
Friday afternoons off now it should be much easier for me till they
did find someone.
The next
Friday afternoon I went to the bank to cash a cheque.
‘Good
morning, doctor,’ the cashier said. ‘The manager said that if you came
in I should ask if you could spare him a few moments.’
My heart
sank. I thought that I was not very overdrawn at the moment but I had
to admit that things were not moving in the right direction. Last
month I had been so short of money that I had had to collect the empty
beer bottles after the mess party so that I could get the deposit on
them back to buy some cigarettes. But I would not take any nonsense;
after all I had only moved my account to the National Provincial in
the first place because the Westminster was being awkward.
‘Yes, of
course,’ I said, trying to sound as though I was not worried, but then
in reality I was not. It simply was not possible to work as hard as I
did and still have the energy left to worry about money!
I followed
the clerk through the doorway into the office. The manager was sitting
solemnly on the other side of his desk. He looked up and smiled
welcomingly.
‘I am so
glad that you had time to come in,’ he said. ‘You gave my daughter her
anaesthetic last Thursday night when she had her baby. I just wanted
to thank you. My first grandchild, you know. Would you care for a
glass of sherry?’
‘Thank you.’
He poured
two glasses of Bristol Cream, and we toasted the health of his
daughter and her baby.
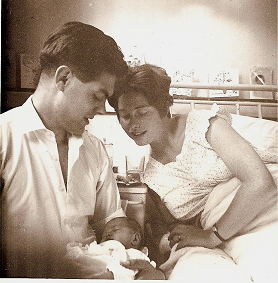
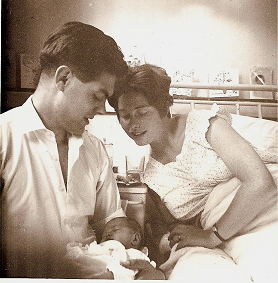
The birth
of our own first child, a fine young boy called Timothy John, was also
the first of many ‘champagne days’ in our married life, though at that
particular time I could not afford even a bottle of plonk; a flagon of
cider from the landlady had to suffice.
When the
12th of June dawned Isabel was already two weeks overdue, though
no-one seemed particularly worried. Of course Isabel was getting fed
up with the wait but she kept her spirits high nonetheless.
That
evening, as I was on call, she spent some time in the residents’ mess
at the hospital. Luckily it was an unusually quiet night. As we sat
watching the television it became quite obvious that Isabel was
getting a lot of strong contractions. ‘Is everything all right?’ I
asked her.
‘Fine, thank
you; it’s just that the Braxton-Hicks are rather strong to-night.’
She was
referring to the normal painless contractions which occur over the
last few months of a pregnancy almost as though the womb was flexing
its muscle in preparation for its real task.
Later she
said
‘I think we
should go home, John.’
‘OK, dear.
I’ll ask Arthur to stand in for me. He said that would be all right if
anything happened.’
We were
about to leave the hospital when the paediatric houseman contacted me.
‘John we are
desperate for a pint of ‘O negative’ blood for a baby that needs an
exchange transfusion and there isn’t any nearer than Bristol. The lab
tells me that you are the only suitable donor that they have on their
books for an emergency like this. Could you possibly let us have a
pint of your blood?’
‘Of course,’
I said. ‘But I must take Isabel home first as she has things to
collect. I’ll come back while she’s packing to give my pint of blood
before I bring her into to hospital to have the baby.’
At least
that was the idea. Unfortunately in my haste to get home to Isabel I
did not lie quietly for twenty minutes after they had taken the blood
off me. It was a mistake! I keeled over before I had taken ten steps
and it was an hour before I was fit to drive. I kept on phoning Isabel
to say that I would soon be on my way, and then phoning her a few
minutes later to say that I was not fit to come.
I did manage
eventually to get her into hospital just an hour before Timothy was
born, but I missed the moment of birth as I was lying down once more
recovering! Who said that women were the weaker sex?
It was when
I got home in the small hours that I opened a flagon of the landlady’s
cider to celebrate my new status as a father.
Now it was
time to think about exams. I swotted for the Diploma in Anaesthetics
of the Royal College of Surgeons examination largely by reading and
re-reading my copy of Synopsis of Anaesthesia but I made a
point of going through the three issues of Anaesthesia for the
year so far. They were fascinating, though there was much that I could
not understand. (For comment on the January issue see chapter 5).
The April
journal began with an article on The control of consciousness which
I found very difficult to follow. The next was on The prediction of
carbon dioxide tension during anaesthesia by a Dr Nunn, who was
research fellow at the Royal College of Surgeons and a consultant
anaesthetist at the Hammersmith Hospital. Although this, too, was
complicated, it was easier to understand.
It is
probable that, from the earliest days, concern has been felt about the
effect of anaesthetic agents upon the gases carried by the blood. In
the eighteenth century ...
I looked
again at the word ‘eighteenth’; what an amazing and unlikely word it
was!
Beddoes
noted the change of the colour of the blood: ‘I thought it might be an
amusing spectacle to see the different tints of blood flowing from a
wound by a leech in consequence of breathing different airs. The
purple from the nitrous oxide was very evident’.
Of course,
the purple blood was nothing to do with the nitrous oxide, merely the
lack of oxygen, and deliberately applying a leech to create a wound
that would bleed was unimaginable. What tough folk those early
researchers were.
In 1847
Mr Hale Thompson of the Westminster Hospital recorded that ‘...under
the full effect of ether, the arterial blood presents it usual
appearance. Nor is there any reason from the inhalation to suppose
that asphyxia can take place, as the usual quantity of air is admitted
to the lungs’.
It was
appropriate that the earliest thoughts should be directed towards the
possibility of oxygen lack rather than to carbon dioxide excess - the
former condition being far more dangerous than the latter ... the
alveolar carbon dioxide concentration is the result of the balance
between production and elimination (rather like the blood urea)...
And a bit
like my bank balance! One day I hoped that I would be producing money
faster than I was spending it. Only last week I had had a letter from
the bank manager pointing out that each month I was spending about £10
more than my pay cheque. While he was not particularly worried by this
he thought that I should bear in mind that one day I would need to
reverse the trend .
Further on
there was a paper about a new drug for premedicating children. It was
called Trimeprazine tartrate, and had antihistaminic, antiemetic and
sedative properties. It sounded marvellous. I would have to try it
out.
I picked up
the July issue and opened randomly. Here was a paper on The
economics of anaesthesia. Apparently in the Southampton group of
hospitals the cost of an anaesthetic was not very much:
...by and
large, I think these figures show a commendable economic modesty on
the part of our specialty. The skill required, the responsibility
involved, the benefit to the surgeon and the patient, let alone the
pleasure derived by the anaesthetist in the giving of a
well-administered anaesthetic, are remarkably cheap at the average
price of £3 13s 9d.
A few pages
on there was a nice little article reporting that halothane and
chloroform did not in themselves alter the oxygen dissociation curve
of blood. As this paper only occupied half a page of text it was a
splendid model of brevity, but as it was only reporting a negative
result I supposed that was fair enough.
Now I turned
to the front pages of the journal; here there was an article from
Newcastle that immediately caught my interest - On the efficiency
of intragastric oxygen. It started:
The
introduction of oxygen into the stomach and intestines of neonates is
widely used in Britain in the treatment of anoxia.
Well, not as
widely as it had been. I knew many people nowadays thought that it was
a poor substitute for ventilating the lungs, but where the skill
necessary for this was not available, no doubt it was still in vogue.
The paper
went on to describe experiments on newborn kittens which proved that
oxygen transfer across the gut could contribute not more than 7% of
the minimum needed for bare cardiovascular survival - I presume they
meant to keep the heart beating. So here was real evidence that
intragastric oxygen could not work But then I never had really
believed it would. I had once wondered whether feeding oxygen up the
ureter might be better; after all the kidney had a huge blood flow
through it and the surface area of the millions of glomeruli was
enormous; of course that was altogether too fanciful.
‘What are
you reading about, John?’ asked Isabel.
‘Oh, about
intragastric oxygen.’
‘Never mind
about that, dear. Supper is ready. Come and have some intragastric
bacon and eggs; it will do you far more good.’
‘That’s
certainly true,’ I replied.
It was the
day before Geoff’s wedding in Rickmansworth. Isabel, four months old
Timothy and I were travelling to Putney where we were going to stay
for two nights. Timothy was going to stop with his Granny while we
went to the wedding on the Saturday. Isabel was eagerly looking
forward to a day off, though she was worried that I would not be
properly dressed since I had refused to hire a morning suit.
‘I am sure
everyone will be in formal clothes,’ she said. ‘You really should get
something from Moss Bros., you know. You will feel very silly if
you’re the only person in the wrong clothes.’
‘Nobody goes
to weddings dressed like that these days, darling, unless they’re part
of the family. Anyway, we can’t afford to hire one. But it will be OK,
my love, you’ll see.’
‘Well. I
hope so.’
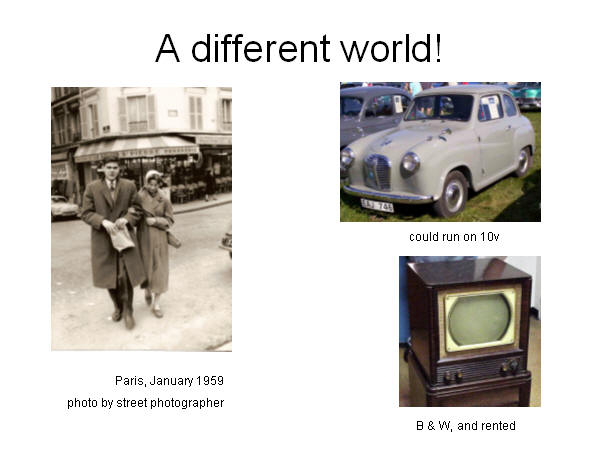
We drove on
across Salisbury Plain. The little car, an Austin A 30, was a real
joy. It was running beautifully on ten volts instead of the normal
twelve. I had discovered only the day before that one of the cells in
the battery was not working properly, and as I had not got the money
for a new battery the mechanic at the garage had put a piece of copper
wire across the appropriate terminals to by-pass the fault. I was
greatly relieved to find it working so well.
‘Shall we
stop at the Linga-Longa restaurant for a cup of tea when we get
there?’ I asked.
‘No. I think
we had better press on while Timothy is sleeping. We’ve a long way to
go. Anyway I don’t fancy the Linga-Longa. The service was very bad the
last time we stopped there.’
‘OK, but my
mouth is very dry. Have you got a peppermint handy?’
I knew that
she had, and I was hoping that the mention of peppermints would put
something else into her mind.
‘Yes, I’ve
got one. Here you are. I think I’ll have a cigarette as well. Would
you like one? I’ll light it for you if you like.’
The ruse had
been successful! Ever since she had become a nurse Isabel had always
had a peppermint after she smoked a cigarette, so that she would not
breathe tobacco all over the patients. I had been smoking heavily
throughout the journey from Taunton and I had not wanted to light
another one on my own in case Isabel thought I was smoking too much.
This way it had become her suggestion not mine. Pavlov would have been
proud of me!
It was three
o’clock before we reached the Upper Richmond Rd and turned into the
drive. The white house looked lovely this sunny summer’s afternoon.
Nostalgic memories flooded through me as I saw the front door, which
was still the bright yellow I remembered as a child.
‘Come on,
John. Don’t day-dream.’
Soon we were
upstairs in the sitting room and my mother was admiring Timothy, her
first grandchild, while Isabel poured out cups of tea.
There was a
knock at the door and the receptionist came in.
‘Your father
wonders if you could give a gas for him in about half an hour. There
is a lady with an abscess who needs a tooth out.’
She paused,
waiting for an answer.
I felt the
adrenaline surge through me. Here I was, an anaesthetist with ten
months experience, who could deal with ill people having major surgery
in the middle of the night, and yet I had not given a simple ‘gas’ for
a tooth extraction in the dental chair since I was a student at Guy’s,
and then I had only done one. I had read all about it, of course,
while studying for the Diploma in Anaesthetics examination that I
planned to sit in November, and I remembered all about the McKesson
gas-and-oxygen machine in the surgery downstairs. As a teenager I had
often gone into the surgery and looked at it, so that I knew exactly
where all the knobs and switches were, but I had not used a machine
like it since I had become an anaesthetist. My father, of course, had
had years of experience with such machines. What was I to say? Of
course I had to say ‘yes’! Otherwise I would look stupid.
The
half-hour turned out to be only twenty minutes, so here I was in the
surgery and the patient on the way from the waiting room.
‘I’ve
switched the cylinders on,’ my father said.
‘I’ll just
check the spare oxygen,’ I replied. Anything to get the feel of the
machine before I used it. I remembered clearly that there was only one
reducing valve for the two oxygen cylinders so first I turned the ‘in
use’ cylinder off and flushed the machine so that the oxygen pressure
fell to zero. By this time the patient had come in and was sitting in
the chair.
‘I won’t be
a moment,’ I said. I turned the full cylinder on, saw the lever on the
pressure gauge rise once more. That’s OK, then. Now turn that one off
and the first one back on again. Good. Right now put the mixture dial
to 0% oxygen and the delivery pressure to 5 mm. Is the nitrous oxide
flowing? Yes, but too fast, so reduce the pressure a bit . Good. One
last look. Be patient, Dad. Yes, the valve on the nose-piece is open
and the machine is close enough to the chair.
The patient
was sitting nervously in the chair now with a prop between her back
teeth and a bib under her chin.
‘I’m just
going to pop this small mask over your nose, Mrs Jones. There that’s
it. Just breathe through your nose now. It will smell rather rubbery,
I expect. Good, that’s right, not through your mouth but through your
nose.’
I pushed the
lever across to the 100% nitrous oxide position, put the delivery
pressure up a bit and at the same time my father held a gauze pack
lightly over her open mouth. She seemed to be going off nicely, I
thought, and I could hear the whistle of the expiratory valve at the
end of each breath. After a few more seconds I moved the mixture lever
to 12% oxygen, put my fingers behind the angles of the jaw and pushed
forwards to make certain the airway was clear. I nodded towards my
father and looked at the patient’s colour. Just a tinge of blue,
perhaps, but nothing to remark about.
‘Thank you,
John. That’s it.’
Good
Heavens, the tooth was out already! I had just been getting into my
stride. I moved the lever to where it said 100% oxygen, which would
cut the nitrous oxide off completely and waited for the patient to
wake up.
‘Well done,
Mrs Jones. Spit into the bowl, please. It’s all over. Your tooth is
out.’
Five minutes
later I was upstairs again drinking a second cup of tea.
‘How did it
go, dear?’
‘Fine, thank
you.’
I did not
mention that I had been nervous. I made a resolve to get some practice
at dental anaesthesia before I came home again. Later my father handed
me two pound notes and a florin.
‘Here are
two guineas, John. It’s your professional fee. Thanks again.’
‘That’s OK,
Dad.’ I replied, and I put the two green notes and the silver florin
in my pocket.
Next day
there were two hundred guests at the wedding. Apart from myself, only
one of the men was not in morning dress. Isabel was very cross with
me.
Geoff and
Liz went away in style on an elephant their uncle had hired from Billy
Smart’s circus.
It was about
this time they made me locum registrar for a couple of months before
finally in October I was conscripted to serve her Majesty the Queen.


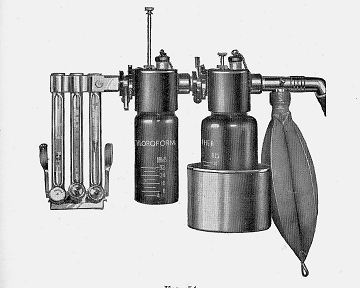
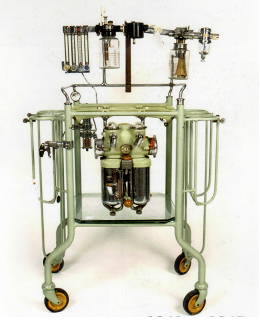
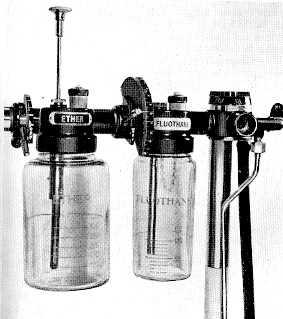 ‘The numbers
are quite arbitrary,’ he explained. ‘But you get to know how far to
move the lever after a bit of practice. It is difficult to tell
exactly what concentration you are using, though it is easy to decide
whether you are giving too little or too much of the stuff; just watch
the patient closely. Of course, how much Fluothane you get from any
given position of the lever depends an awful lot on how long the
vaporizer has been switched on; after a few minutes the Fluothane gets
amazingly cold and the gas that flows through it does not pick up so
much vapour.’
‘The numbers
are quite arbitrary,’ he explained. ‘But you get to know how far to
move the lever after a bit of practice. It is difficult to tell
exactly what concentration you are using, though it is easy to decide
whether you are giving too little or too much of the stuff; just watch
the patient closely. Of course, how much Fluothane you get from any
given position of the lever depends an awful lot on how long the
vaporizer has been switched on; after a few minutes the Fluothane gets
amazingly cold and the gas that flows through it does not pick up so
much vapour.’ The
main theatre (general surgery, urology and gynaecology) had two tables
in it, often with two different surgical teams working side-by-side.
There was no delay between cases because the next patient was
anaesthetised before the previous operation was completed. The speed
of surgery was remarkable - the senior surgeon completing two
cholecystectomies and a prostatectomy inside an hour, while a locum
consultant, who incidentally had taught me anatomy at Cambridge, was
painfully slow. There was also a theatre for ENT surgery, and another
in the maternity department. Orthopaedic and eye surgery were done at
East Reach Hospital across the town; the casualty department was there
too.
The
main theatre (general surgery, urology and gynaecology) had two tables
in it, often with two different surgical teams working side-by-side.
There was no delay between cases because the next patient was
anaesthetised before the previous operation was completed. The speed
of surgery was remarkable - the senior surgeon completing two
cholecystectomies and a prostatectomy inside an hour, while a locum
consultant, who incidentally had taught me anatomy at Cambridge, was
painfully slow. There was also a theatre for ENT surgery, and another
in the maternity department. Orthopaedic and eye surgery were done at
East Reach Hospital across the town; the casualty department was there
too.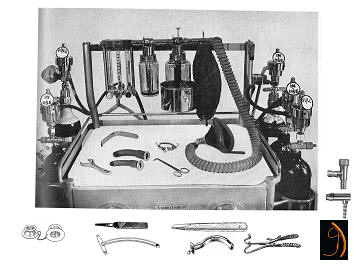


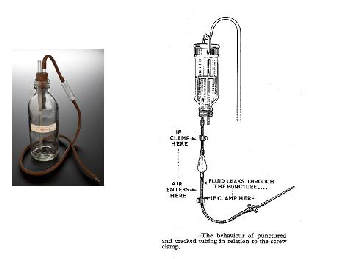 and the rubber tubing used for intravenous infusions from glass
bottles. If this tubing was perished at all There was danger of
unnoticed air embolism.
and the rubber tubing used for intravenous infusions from glass
bottles. If this tubing was perished at all There was danger of
unnoticed air embolism.  There was no automatic provision of suction in the anaesthetic room,
though it could be arranged if necessary; otherwise swabs did the
trick. At the end of the operation new tubing for the anaesthetist was
put onto the electric suction machine the surgeon had been using.
There was no scavenging of expired gases and vapours, no mechanical
ventilators, and no recovery ward, though patients were usually kept
in the corridor outside the theatre for a few minutes, looked after by
the nurse from the ward.
There was no automatic provision of suction in the anaesthetic room,
though it could be arranged if necessary; otherwise swabs did the
trick. At the end of the operation new tubing for the anaesthetist was
put onto the electric suction machine the surgeon had been using.
There was no scavenging of expired gases and vapours, no mechanical
ventilators, and no recovery ward, though patients were usually kept
in the corridor outside the theatre for a few minutes, looked after by
the nurse from the ward. 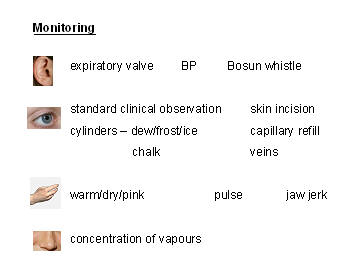
 just checking!
just checking!