2. ETHER AND ETHYL CHLORIDE
Diethyl Ether. H5C2-O-C2H5. A colourless flammable volatile liquid with a pungent smell and an irritant vapour.
Ethyl Chloride. C2H4Cl. A colourless flammable gas with a pleasant ethereal smell and a burning taste.
Putney, London
I had a small operation early in 1936, just before my second birthday. I was probably given ether at the time, and perhaps ethyl chloride too. Of course, I cannot be sure about the anaesthesia[1], though I am certain about the surgery.
I had had several bouts of what my mother called ‘septic throat’ in the first half of the year, and now, just after my fifth birthday the doctor was again shining a torch into my mouth.
‘Open wider, there's a good boy. I'll just press your tongue down like this so that I can see the back of your throat.’
I gagged as the wooden spatula touched the sensitive part at the back of my tongue.
‘It's all right now, John, I've finished,’ the doctor said, and turning to my father he continued ‘this young man's tonsils are huge, Jack, and they are chronically infected. It is no wonder that he is getting these sore throats all the time. We had best have them out, you know.’
The conversation between the two men continued for some minutes but I was not listening to them. Have my tonsils out, eh? I was not sure exactly what tonsils were, but if they had to come out that was all right so long as they saved them for me. I didn't want bits of me thrown in the dustbin before I had had a chance to look at them properly.
That afternoon I discussed it with my mother.
‘Will they keep my tonsils for me, Mummy?'
‘If you really want them to, dear,’ my mother replied, anxious to keep me happy. ‘I'll ask the doctor. You will have a present as well if you're a good boy.’
‘A present? What is it, Mummy? Tell me, tell me. What is it? Is it a train?’
‘It's a 'wait-and-see present' so you will just have to wait and see.’
A few days later my mother took me to the nursing home in Carlton Drive, where they persuaded me with some difficulty to get undressed and climb into a bed, but I was adamant that I would not take the small orange capsule that they offered me.
‘I don't like it. I don't want it. I won't have it.’ And I wouldn't.
They tried cajoling me, but without success. So next they tempted me by taking the powder out of the capsule and putting it in a teaspoonful of strawberry jam. I took this eagerly. I did like strawberry jam! But ugh! I spat it out quickly.
‘It's horrid,’ I cried. ‘It's horrid!’[1]
‘John,’ said the nurse when I had calmed down, ‘let me put the powder on a spoon, without the jam, and just tip it at the back of your throat so that it goes down without touching the sides? That way you won't taste it at all.’
Reluctantly I agreed to try it. The manoeuvre was entirely successful in that the powder was swallowed, but I complained that I had still tasted it a bit.
‘Never mind. I'll read you a story.’
The next thing I knew there was a soreness in my throat and a muzziness in my head and a funny smell like the glue you used to stick model aeroplanes together, though I couldn't think what it was called[2].
‘It's all over, John,’ said a distant voice. ‘It's all over.’
‘My throat hurts.’
It felt as though someone had been rubbing sandpaper over it. The tears ran from my eyes and then I retched which made it worse.
‘We'll give you some jelly and ice-cream[3] later on, and that will soothe it for you. Just go back to sleep again, there's a good boy, and it will be better soon.’
When I next awoke my throat was still painful but not quite as bad as before.
‘Did they save my tonsils?’
‘Yes, they did. You can see them later.’
‘Why can't I see them now?’
‘Mummy will be here soon. She can show them to you.’
‘I want to see them now.’
The nurse sighed. She might just as well give in! I was both fascinated and repelled by my tonsils when I saw them. They were floating around in a small jar of fluid looking rather fluffy and somewhat useless like two meatballs left over from lunch. Surely they ought to look better than that? Still they were very interesting, and they had been a real part of me hadn't they?
‘Look, Mummy, here are my tonsils.’
‘Yes, darling. Very nice, but put them away now, please. There's a good boy.’
‘Don't you like my tonsils, Mummy?’
‘I have already said that they are very nice, haven't I? But I've seen them now so just put them away.’
I was disappointed that she wasn't as excited about my tonsils as I was, but grown-ups were funny about things, weren't they? The long-awaited present was produced. A lovely red clockwork car. I was very pleased with it.
Later in the day they did give me some ice-cream and it was soothing as they had promised. Then they tried to settle me down again for the night. A new nurse had arrived and she sat in a chair in the corner of the room.
‘What's that lady doing there?’ I asked the nurse that I already knew but who was about to go home.
‘She is just going to sit there quietly to make sure everything is all right. You just go to sleep now, John. There's a good boy.’
‘I don't like her. Tell her to go away.’
My throat was hurting again and I felt like making a fuss. Eventually they said the nurse would go away but they didn't fool me. I knew she was sitting in the corridor just outside the door. I had been shown earlier how to ring the bell by pressing the little button, so I pressed it. Another nurse arrived.
‘She's still there,’ I said to her grumpily as I fell into a deep dreamless sleep.
Betton, Shropshire
The war was not yet finished but the allied troops were storming across the continent and everyone knew that it could not be long before the Germans were beaten, serve them jolly well right!
At my boarding school near Shrewsbury we would sometimes be playing cricket on a summer's afternoon when the Boeing bombers, or ‘Flying Fortresses’ as they were called, and the Lancasters and Halifaxes started to cross the sky on their way to bomb German cities. They came in sorties of eight planes at a time (or was it twelve?). As one group faded into the distance so another would be noisily overhead and a third would be looming into view on the opposite horizon. An awe-inspiring spectacle that brought home to us the enormity and horror of the war, especially as three hours later the planes were still droning across the sky on their way to bomb Germany.
At the end of term some of the boys, and I was amongst them, would travel to Paddington on the Great Western Railway. What an adventure! The week before we left we were busy making graphs of the journey, plotting time against distance. The broken line, which was drawn in while still at school, showed the journey as predicted by the timetable in Bradshaw's railway guide. On the journey itself we carefully plotted what actually happened and joined the points up with a continuous line. It was tremendous fun... Didcot... expected arrival 12.03, expected departure 12.09... actual arrival 12.25, actual departure 12.32. It was all entered precisely. Between stations we calculated predicted average speeds from the timetable, and then timed with stopwatches how long it took to pass between the mile markers at the side of the track. I found it all very exciting and I enjoyed the journey immensely.
There was only one thing that spoilt it... my wretched knee! It was not really the knee itself which was bothering me, it was the itchiness that had developed where the plaster had been. I couldn't stop myself from scratching it. If only I had got something which would get the sticky stuff from the plaster off my skin perhaps it would be better. When I had first removed the elastoplast I had tried to get the white stuff off by washing it and scrubbing it but it just wouldn't budge. Now there was a thick dirty black line around the new pink skin where the graze had healed and it was itchy and getting spotty as well. It would be all right when I got home, my mother would know what to do!
‘I usually use nail polish remover to get that off, dear, but I haven't got any at the moment,’ she said. ‘Have you got anything that would do it, Jack?’
My father nodded. ‘Yes, there's some ether in the surgery. I'll bring it up. Soon he was back with a brown glass bottle. He poured some of the clear liquid it contained onto his handkerchief and gently rubbed the skin. It was amazingly cold, though I didn't know why that should be. Perhaps it was because it evaporated so quickly. The black sticky stuff came off my knee at once[1] but left a dirty mark on the handkerchief.
‘Thanks, Dad. That's a lovely smell, isn't it?’
‘Yes, it's all right in small amounts but it makes you cough if you breathe too much of it. It'll put you to sleep as well, you know, if you breathe it for several minutes.’
Oh, I thought, how strange. Put you to sleep, eh? I wonder how it does that.
‘Mum,’ I said, ‘I'm hungry. Is there anything to eat in the fridge?’
Clare College, Cambridge.
We were learning about the heart, the blood vessels and the circulation of the blood in our physiology lectures and demonstrations. I had always been interested in blood and how it moved around the body ever since the day Sheila had shown me, when I was six or seven years old, what happened if I put one arm straight up in the air and let the other one hang down. If I waited for a minute, then suddenly put my two hands side by side in front of me they looked quite different, one being pale and empty of blood and the other one red and full of blood, with the veins standing out like blue string. I used to marvel at it.
A few years later, when I was ten, I had discovered the pulse in my left groin; I had thought for a day or two that there might be something terribly wrong with me. I knew about the pulse at the wrist, of course, as Dr Chisholm always counted it carefully whenever he came to see me because I was ill. But a pulse in the groin was another matter. I was not sure whether to be relieved or more worried still when I found I had a pulse in my right groin too. Still, as I felt fine, and I had not died in the two days since I had made the discovery, I guessed it was all right.
Then when I was fifteen we had dissected pithed frogs and cut out their hearts, which continued to beat normally for an hour or so after we put them into a fluid called ‘Ringer-Locke’s Solution’, which tasted salty like blood when you sucked a cut finger. It was really strange to see a heart beating in a jar all on its own. The zoology master had also shown us how to demonstrate the direction that blood flowed in our veins. He had held his right arm out pointing slightly downwards so that we could see the veins on his forearm; then he had put the forefinger of his left hand onto one of the veins and then had swept his middle finger along the vein towards his elbow so that it was emptied of blood. We could see the slight groove that was where the bulge of the full vein had been. It was not until he had lifted his forefinger that the vein filled again and we could see clearly that the blood was running up his forearm and not the other way.
That day we dissected the frogs I noticed that while mine was a male frog the boy next to me had a female frog. I suggested we cut out the ovary from the one and the testis from the other, chop them up and mix them. So we did just that, keeping the result in a jar of water. Imagine our delight and surprise when a few days later there were four little tadpoles swimming around in the pot. Unfortunately they all died within another 48 hours [1a].
Now we were learning all about it in much greater detail. When we had arrived at the start of the term one of the books they recommended to us was Applied Physiology by Samson Wright. I had gone to Bowes and Bowes, the splendid book shop, and had spent thirty shillings on it. I was very proud to have it on my shelf.
As I was leaving school one of the masters had said to me ‘Now remember, when you are at University you should do eight hours studying every day of the term. Yes, eight hours every day! That includes lectures and your own private studying. If you do that you will get as good degree and still have time to enjoy yourself as well. It is only by being self-disciplined that you will be able to manage it but it is absolutely essential. Remember, now, eight hours.’
Of course, that was a load of nonsense. I had never had to work for any exam and I was not likely to start doing it now.
Still that evening I opened my new book and turned the pages till I came across the chapter on Heart and Circulation. It was difficult to understand unless you read it very carefully.
Here was something about the pulse:
Arterial Pulse.- The blood which is thrown into the aorta during systole....
‘Thrown’, eh? That was a nice way of putting it, but I wondered if it was correct usage of the word?
.... is accommodated partly by moving the entire arterial column on at a greater velocity, and partly by stretching the arterial wall. This increase of pressure and this arterial distension are transmitted from one segment of an artery to the next, in the form of a wave - the pulse wave - which is independent of the velocity of the blood flow... the velocity of the pulse wave is considerably more rapid than that of the blood.
So the pulse wave reached the wrist quicker than the blood did? That was amazing! I supposed that it was rather like throwing a stone into a pond; the ripples moved outwards in circles even though the water itself was not really moving outwards. I read on;
Circulation Time.- By this is meant the time for the blood to travel from one point in the circulation to another. It is thus a measure of the average linear velocity of the blood flow which is directly related to the cardiac output.
I thought about that for a moment; the more blood that the heart was pumping out each minute the quicker the blood would be flowing, and therefore the shorter the time it would take to travel any particular route or distance. It was obvious really but the first time one read it it was not instantly clear. I guessed that the more one read about physiology the easier it would become, but it was all so new at the moment. The paragraph went on to describe how the circulation time could be measured by injecting various things into the blood stream.
The substances commonly used are:
1) Decholin (Na salt of dehydrocholic acid)...
I knew that the word ‘choleric’ meant ‘full of bile’ so I guessed that this was one of the bile salts, and I was not surprised when the paragraph went on
when the drug reaches the mouth and pharynx it gives rise to an intensely bitter taste and smell. The ‘arm to tongue’ circulation time is the interval which elapses between the injection to the first recognition of the bitter taste[1].
It continued:
2) Sodium cyanide...
Cyanide! That sounded very dangerous.
On reaching the carotid body the chemoreceptors are stimulated and send up excitatory impulses to the respiratory centre. The end point is dilatation of the alae nasi followed by a deep inspiratory gasp and 6-10 rapid breaths. This gives the ‘arm to carotid’ time[2].
3)Magnesium Sulphate...
Magnesium sulphate? I knew that magnesium sulphate was the chemical name for Epsom salts and it surprised me that you could inject it into a vein. I had always thought that it was a laxative!
on reaching the throat there is a sudden start combined with an intense feeling of heat in the pharynx; the heat is progressively felt in the face, hands and finally the feet. The sensation passes off in 10-20 seconds. This gives the ‘arm to hand’ and ‘arm to feet’ time[3].
That didn't seem very pleasant!
4) Ether...
Ether? What an amazing list this was turning out to be!
... 5 minims[4] of ether (in an equal volume of saline) are injected intravenously. When the ether reaches the respiratory passages it produces a gasp. a cough, and a grimace, and ether can be smelt in the breath. This gives ‘the arm to lung’ time... normally 3-9 seconds.
Yes, that was a truly amazing list: a bile salt, a poison, a laxative and an anaesthetic. It was difficult to believe.
A.D. 1955
Guy's Hospital, London.
I was feeling extremely nervous as I walked into the casualty department, even though two of my group of students had already spent a day there, and had thoroughly enjoyed it. I was feeling insecure because I was uncertain what would be expected of me. The prospect of helping the doctors and nurses to deal with the patients was certainly exhilarating, but daunting too. After all what did I know about illnesses and accidents, poisonings and appendicitis? Nothing. Nothing at all. It would never do to admit it to anyone, of course, though the experienced people in the department would know that it was my first day, and they would expect me to be entirely ignorant and stupid. So what the hell? But I was nervous nonetheless.
As I walked through the door I saw with relief a face that I recognized. It was Bob who had been the houseman on my last ‘firm’ and who was now one of the new casualty officers. I walked up to him.
‘Hello,’ I said shyly, ‘I'm on casualty this morning. What should I do?’
‘Ask Sister which is the next patient, and take him into one of the cubicles and find out what the trouble is. Then come and tell me all about it, and we'll go and see the patient together. OK?’
‘OK.’
The next patient in the amazingly long queue was a middle-aged man with a nasty boil on the back of his neck.
‘That looks very painful, Mr. Legg. How long have you had it?’
‘About a month ago. It started as a pimple that wouldn't go away, and then a week ago it began to get bigger. It is certainly bloody painful.’
‘Have you had any other boils recently, or is this the only one?’
‘It's the only one. I've not had a boil since I was a boy, and that was on my backside.’
We both laughed.
‘Just wait here and I'll go and tell the casualty officer about it,’ and I went to find Bob.
‘That boil needs the pus drained out of it, Mr Legg,’ said Bob when he saw it. ‘If you will just be patient for another few minutes we will see to it. We'll spray it with some special cold liquid which will freeze it so that it won't hurt.’
Outside the cubicle, and out of Mr Legg's hearing, Bob explained what he wanted me to do.
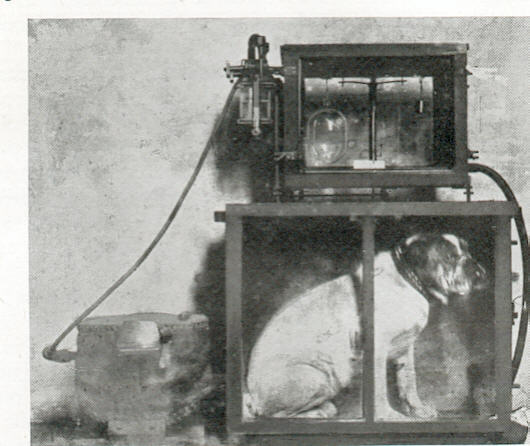
‘Here's a bottle of ethyl chloride. You need to tip it upside down and press the lever like this. You can see how the liquid comes out of the nozzle in a fine jet. When it hits the boil it will evaporate and cool it down as it does so. If you spray long enough it'll freeze the top of the boil so that you can stick a scalpel blade in it without it being too painful. Do you think you could do it? There's a lot of other people waiting, and it would save some time if you think you'd manage it all right. It's simple enough.’
‘I'll have a go,’ I said, rather doubtfully.
I spent several minutes collecting together the things I thought I would need.. sterile swabs, a dish to put them in, a scalpel and some elastoplast. The treatment room at the end of the corridor was empty and it seemed the right sort of place for the task, so I took Mr Legg down to it. I asked him to lie on the couch on his stomach with his arms up and his forehead resting on his hands.
‘Are you comfortable like that?’
‘Yes, thank you.’
‘I'll just spray this onto your neck then,’ and I pressed the small lever. I watched, quite fascinated, as the thin jet of clear fluid hit the red swelling and frosted it over. I wondered how long I should continue with the spray. After a minute or so the boil still didn't look frozen enough for me to stick a knife in it, so I persevered for another whole minute. By now the skin over the boil was icy white and it seemed likely that it was truly frozen. Just as I stopped the spray Mr Legg slumped on the couch completely unconscious. I thought that he must have fainted. Perhaps the smell and the heat had done it. I looked around anxiously as though something in the room would give tell me what to do. Thinking that at least I had better let the pus out, I picked up the scalpel and thrust the blade into the pointing boil. A gush of blood-stained creamy fluid poured out of the incision I had made. Mr Legg did not stir. Half minute later he began to moan as he recovered consciousness.
‘Are you OK, Mr Legg? I think you must have fainted with the heat and all the strange smells. I'll open the window and let some fresh air in. There, that's better isn't it? Don't get up yet. I'll just put a dressing on the boil.’
‘I've got a terrible headache.’
‘It will get better in a moment,’ I said, sounding more confident than I was feeling. ‘Just lie still for a few moments and I'll get Dr Jones to look at you before leave the hospital. I went off find Bob.
‘Good Heavens, you must have anaesthetised him with the ethyl chloride. Did you know that it was a general anaesthetic?’
‘A general anaesthetic?’
‘Yes. They use it all the time in the ENT theatre. They give it to the children before they get the ether going - you know when they have their tonsils out. It's very powerful stuff.’
‘Oh,’ I said.
‘It's a good thing that he wasn't lying on his back or he might have obstructed his airway with his tongue. Would you have known what do?’
‘No.’
‘Thank God that it didn't happen then, or we would have been in real trouble. It doesn't bear thinking about. Let me look at him and make sure that he's OK.’
Luckily Mr Legg seemed fully recovered, and half an hour later he left the hospital none the worse for his adventure[1].
When I got home that night I sought out my father's old book on anaesthesia. It was in exactly the same place on the same shelf in the bookcase as it had been all those years ago when I had read about chloroform. When I took the book out this time I paused at the title page and studied it more closely than I had before:
Essentials of
GENERAL ANAESTHESIA
With Special Reference to Dentistry
By R.R.MACINTOSH,
M.A., M.D., F.R.C.S., D.A.
Nuffield Professor of Anaesthetics, University of Oxford; Late Anaesthetist and Lecturer in Anaesthetics, University College Hospital Dental School, Assistant Anaesthetist, Guy's Hospital Dental School.
and FREDA B. PRATT, M.D., D.A.
First Assistant, Nuffield Department of Anaesthetics, University of Oxford, Late Clinical Assistant in Anaesthetics, University College Hospital Dental School.
Fancy that! Professor Macintosh once had worked at Guy's, and both I and Dr. Pratt had been at the Dental School at UCH. What a coincidence! It was only two years ago, during the summer vacation from college, that I had worked for five weeks as a porter in the Dental School at UCH, and here I was now a clinical student at Guy's, and, of course, my father had been a dental student at Guy's as well during the first World War. A remarkable coincidence. I turned the page.
Here it was:
Chapter XVI. Ethyl Chloride . . . . page 150.
I quickly found the chapter and started to read it:
The boiling point of ethyl chloride (C2H5Cl) is 54.4oF. At ordinary room temperature and pressure it is therefore a gas, but the increase in pressure required to liquefy it is so small that it can be kept with safety as a liquid in glass containers. It is supplied in bottles of convenient size and shape from which it can escape through a nozzle when the control lever is depressed.
There was a picture showing the bottle and it was just like the one I had used earlier in the day. I glanced further down the page.
Ethyl Chloride burns with a blue flame, but it can be used safely in a room with an open flame.
I had not known that it was inflammable when I had been using it, though it did not sound too dangerous. At the bottom of the page it said:
Ethyl Chloride is a potent anaesthetic agent. Its advantages are:
1. It is not unpleasant to inhale.
2. It is easy to administer.
3. It is economical.
4. It is easily portable.
5. Induction of anaesthesia is rapid.
6. The signs of anaesthesia are simple and well defined.
It continued on the page opposite
The disadvantages of ethyl chloride are
1. Nausea, vomiting, headache and prostration frequently occur after deep or prolonged narcosis.
That did not sound too pleasant. Mr Legg, my patient in the casualty department, had had a headache all right but it had not lasted for long, thank goodness, and he certainly hadn't been sick, and neither had ‘prostration occurred’.
2. The stages of anaesthesia are passed through so rapidly that it is easy to administer an overdose.
Well, I had not given Mr Legg that sort of an overdose but he certainly had gone to sleep amazingly quickly.
3. Involuntary micturition and even defaecation are more liable to occur under anaesthesia than with other agents.
Ugh, what if that had happened! It would have been much more awkward.
The stages of ethyl chloride anaesthesia can be conveniently divided into three: induction, surgical anaesthesia, and overdose.
Well, that was simple enough!
I flipped through the next few pages until my eye was caught by a delightful photograph of a little girl sitting a dental chair.
Underneath it said :
Great Ormond Street method of giving ethyl chloride.
I wondered where the girl was now and what she was doing. Of course, I would never know.
Further on in the book there were pictures of the mask that the anaesthetist had been using in this photograph. It was called a Schimmelbusch mask, and consisted of an oval-shaped metal frame, some three inches wide by four inches long and shaped like half an egg. Before use it was covered with two layers of gauze.
It was some weeks before I saw ethyl chloride used in earnest in the operating theatre. It was quite amazing.
The patient was a young boy of six who was going to have his tonsils and his adenoids removed. He had been given a barbiturate called Nembutal (pentobarbitone) an hour and a half earlier in the ward. The dose of 0.6 grain per stone of body weight had been very effective, and the boy was sleeping soundly when he reached the anaesthetic room.
The anaesthetist took a Schimmelbusch mask, already covered with gauze, and held it close to the boy's face, but not actually touching it. He explained to me that the ethyl chloride was really a gas at room temperature but it liquefied very easily if compressed, so that it was possible to keep it as a liquid inside a thin glass tube. He pressed the lever at the end of the tube, just as I had done in the casualty department, and let a short jet play onto the gauze.
‘You must listen to every breath the child takes. If he holds his breath at all you must stop the spray until he starts again, or he'll get an overdose. It's a very potent anaesthetic, you know.’
It smelt rather different from the last time; more like a perfume, really. I was about to comment when the anaesthetist said:
‘They've put some eau-de-cologne in it so that it won't be so unpleasant for patients to inhale.’
So that was it. I was reminded of the '4711' I used to buy at Woolworth's for my mother's birthday when I was in my early teens. At least that had been better than the revolting musk perfumes so many women wore these days!
‘It's time to change over to ether now,’ said the anaesthetist. He put down the glass tube containing the ethyl chloride and picked up a brown rectangular bottle labelled DIETHYL ETHER. He tipped this sideways so that drops of clear fluid fell onto the gauze from the fine metal nozzle that stuck out of the cork at the top of the bottle.
After a few further breaths he lifted the mask briefly and put a large piece of gamgee with a hole in it over the child's face. The hole left the mouth and nose uncovered but the eyes and the rest of the face were hidden. The mask was put back again and the drip of ether re-started.
‘Ethyl chloride is much less irritating to breathe than ether, but it is much more powerful... and dangerous[2]. So we only use it to take the patient down deep enough to breathe the ether without coughing and spluttering. Sometimes you need to change the mask as the gauze gets so cold it stops the ether evaporating properly, though it seems all right this time.’
‘How did you know that it was time to change over to ether?’
‘By watching the breathing. Did you notice that it was rather irregular at one stage when he was getting the ethyl chloride? Then it became quite regular, both in depth and in rate. Well, at that stage he was in surgical anaesthesia. I waited a moment or two longer to be sure he was deep enough, otherwise he might have come round too quickly when I stopped the ethyl chloride and before we had got the ether into him. Sometimes I put a second piece of gamgee with a hole in it over the top of the mask so that the patient has to breathe through the gauze where I am dropping the ether. Still, as I said, it seems to be all right this time.’
And so it proved. The boy had some sort of metal blade put in his mouth and his tonsils were in the dish on the instrument trolley almost before I could take in what was happening. He went and went back to the ward, spitting blood and saliva, and tearful with it.
We were on Addison[1] ward, standing at the foot of the bed of a new patient with had been admitted with a two day history of severe asthma. The poor woman was fighting desperately for each breath. She looked totally exhausted by the effort of it all.
‘Perhaps, they should call in the psychiatrists,’ said Bill.
‘Call in the psychiatrists? Why would they want to do that?’
‘Well apparently sometimes they can stop an asthmatic attack by hypnosis. I saw them try it once.’
‘Did it work?’
‘No, not the time that I saw it, but the psychiatrist said he had had a couple of amazing successes in his time, and it didn’t do any harm.’
‘No, I suppose not.’
‘I once saw someone do a stellate ganglion block for status asthmaticus,’ Harry chipped in.
‘Stellate ganglion block? Did that do any good?’
‘No, none at all, and it looked pretty hairy to me, what with sticking a long needle into the bottom of the neck and hoping you didn’t hit the top of the lung.’
‘Gosh, that sounds terribly dangerous.’
‘Yes, a pneumothorax is the last thing you would want if you had bad asthma, but apparently it has worked on some occasions.’
In the event the physicians were sufficiently alarmed by their patient’s deteriorating condition, that they called in Dr Rink, one of the anaesthetists, to try the effect of ether on her. He arrived pulling an anaesthetic machine behind him.
‘Hello, Mrs Brown. I am Dr Rink. I am just going to give you something to breathe that will make you very sleepy, and it will help get rid of your wheezing. I just want you to breathe from this mask. There, that’s good. It’s just oxygen at this moment. There, you are beginning to get used to it already, aren’t you?’
He sounded so calm and reassuring that she seemed to be getting better even before he turned the ether on.
‘There, that’s good. Now you will notice a new smell,’ and he lifted the lever at the side of the ether bottle just a fraction, and then half a minute later, he moved it a bit further. It must have been four or five minutes before the lever was fully raised. I could see the surface of the ether being ruffled by the oxygen flowing across it, even though the plunger was still at the top. I remembered all the coughing and spluttering the last time I had seen ether used. It was fascinating how well everything was going so well this time.
Dr Rink started to lower the plunger, taking it so slowly again.
‘Ether is a powerful bronchodilator,’ he said to us, ‘and it is a respiratory stimulus too in light anaesthesia, which is just what you need.’
He pulled back one of her eyelids, so that he could see the size and position of her pupil.
‘She’s getting nicely deep now, but we’ll take her even deeper. We’ll keep her asleep for fifteen minutes or so, and then we’ll let her wake up again. I think her wheezing is a little less.’
‘Did you give her any atropine?’ I asked.
‘Oh, yes, just a little’ he replied. ‘If you don’t give any at all, you get such a lot of saliva, even though she is so dry. I know she’s been too breathless to drink much these last two days, and she’s been mouth breathing as well, but it doesn’t stop her salivating when you give her something irritant like ether to breathe. Unfortunately atropine does dry the bronchial secretions as well, which is a pity as we would like them to be thin and loose so she could cough them up easily, so I just gave her 1/200 of a grain, which helps a lot, but doesn’t overdo it.’
‘Can I listen to her chest ?’
‘Yes, do. You can tell me if it is any better.’
I put my stethoscope on her chest just below her clavicle. I could hear the air - well, the oxygen and ether - getting into her lungs much better than it was before, and though there was some still wheeze it was dramatically reduced.
Fifteen minutes later he turned the ether off, and we turned the lady onto her side. We watched her for ten minutes or so, and then she started to cough up some phlegm.
‘Well, she couldn’t do that before, could she?’ said Dr Rink. ‘And she is clearly breathing easier than before. Let me know how she gets on, will you?’ he added, turning to the houseman.
‘Of course.’
Though I thought that perhaps some of the wheeze did return as she woke up, it was still very much better than it had been before. She retched several times during the next hour, but then demanded something to drink. The nurses gave her iced water.
Over the next day she improved beyond recognition. The medical registrar said it was because the steroids were taking effect at last, but I was convinced that it was the ether that had done the trick!
I found my first day as a houseman utterly nerve-racking. I was alarmed at how little I knew and furthermore how little I understood what was expected of me. Did I really have to cope with everything that came my way, or was I allowed to ask for help when I was in doubt? If so, whom was I to ask? There wasn't anybody! The senior registrar seemed too aloof and important to bother and anyway he was busy doing a locum consultant job at St Mark’s three days a week. The senior of the house officers was attached to the senior of the two surgeons that made up the ‘surgical firm’. He was too busy with the ‘major take’ to worry about me. My emergency admissions in these first three months would be limited to the infected cases that needed surgery; certainly there would be quite a few of those but somehow it was not as exciting as the ‘real stuff’.
I arrived at eight o'clock, unnecessarily early as it happened, but at least it enabled me to be sure that I would not be late. I knew the nurses would not be pleased to see me on the ward before nine o'clock so to pass the time, and to prepare myself, and to calm myself too if possible, for I was very nervous, I pulled out of my pocket the two sheets of paper on which the previous house surgeon had written details of the ward patients. This proved a most useful piece of paper since at Guy's the housemen were not expected to write the notes themselves; this task was the specific duty of the medical student to whom the patient had been allotted. True there was a small space reserved at the side of the treatment card where the houseman could make telegrammatic notes for his own use but these were often indecipherable to anyone else.
There were fourteen patients altogether, eight men and six women, each surgeon having only a very limited number of beds allocated to him. This was only about half the number held by the surgeons at the outer hospitals in the district; new house surgeons at Lewisham and New Cross to-day would perhaps be taking over the care of twenty-eight or thirty patients. I was nervous enough as it was. That many would be terrifying!
The first patient on the list happened to be an old friend of mine. In my first few weeks as a student at Guy's I had ‘clerked’ him in as an emergency with colicky pain in his right hypochondrium. It seemed so obvious now, exactly three years later, that the poor man had got biliary colic, but for some inexplicable reason the surgical registrar on duty at the time had got it in his head that the old man was hysterical. It had taken the poor old boy all of the three years to convince people that he genuinely needed help, and finally last week, on his fifth admission to hospital since 1952, he had had his gallbladder out and his common bile duct explored to remove the stones that were giving him such pain. He was a great character. He owned a fruit and flower stall on the approach to London Bridge Station. He would often stop me on my way to the station to show me the seven or eight watches he wore up his forearm, and he would produce a thick wad of beautiful white five pound notes from his pocket to demonstrate that he was a man of some substance.
‘I've got plenty of money,’ he would say, ‘plenty of money.’
I used to buy wonderful bunches of dark red or pale pink or bright yellow roses, still in tight bud, from his barrow (two shillings a dozen) to give to Isabel. Often too I would see the old man outside the hospital with a huge bunch of flowers in his hand that he was taking to Sister Falwasser, who had nursed him on Job ward. Now he had had his operation and had got over it well. He should be going home in another week or so[1].
As I walked round the wards getting to know the other patients I kept a careful watch on the groups of coloured lights which were scattered around the ceilings of the hospital. These were the means by which the housemen knew when someone was trying to contact them. I wondered who would be the first person to contact me.
In the middle of the morning, while I was talking to a lady who had had a hernia repaired three days earlier, my combination of coloured lights duly came up, the red flashing, the green and yellow steady. I phoned the porter's lodge. Front surgery would like me to phone. Front surgery said ‘hang on a moment, please’ and then another voice told me that there a patient who had had a bowel resection for cancer by my boss one month ago who now had a vaginal discharge and please would I come and see her. Apparently the operation had been very extensive and had included a hysterectomy. I said I would come straightaway. A vaginal discharge? What on earth could be causing that?
When I got to Front Surgery one of the nurses led me to where the patient, a pleasant woman of sixty, was sitting. I arranged for the nurse to stay while I examined her. I put the speculum carefully into place and there to my amazement was a surgical swab at the vault of the vagina. I picked up the Vulsellum forceps and removed it. Fancy that! It must have been put there at the time of the operation and not been removed at the end.
‘I think things will be better now, Mrs Harris,’ I said without any explanation.
‘Thank you, doctor.’
Amazingly she did not ask any questions at all but just took my word for it. I was overawed by the trust she appeared to have in me. Pleased as I was to have passed the first hurdle I decided not to tell my consultant boss about it. Let sleeping dogs lie. I wrote a short comment in the lady's notes and went back to the ward to see the rest of my patients. One of them had just died. It was not in any way an unexpected death as the old man had had severe pneumonia after an operation for perforated gastric ulcer which had proved to be malignant. They had been giving him ‘Brompton cocktail’ for the last three days.
‘Mrs Jones would like to talk to you if possible, doctor,’ said the staff nurse. ‘She is very upset even though she knew it was going to happen.’
‘I'll talk to her now. Where is she?’
I sounded more confident than I felt but it was the least that I could do for the poor old lady.
‘She is in Sister's office.’
I made my way to the office at the end of the ward.
‘Hello, Mrs Jones. We are all so very sorry about your husband. He was a fine man.’
I paused searching for some words to comfort her. She looked up and said in a firm voice
‘Would you cut his wrist for me, doctor? So that I will know he really is dead. Would you do that for me? I promised him I would not bury him without cutting his wrist first.’
I looked at her in amazement. Cut his wrist? Cut his wrist! I had read once long ago about that being done by some people somewhere in the world but I could not remember where or when. People just wanting to be sure that their loved ones were really dead. But I had never expected to be asked to do it. I looked at the poor sad woman and made what seemed the only possible decision. After all it could not possibly do the poor man any harm.
‘All right, Mrs Jones, I'll do it for you if you are really sure that is what you want.’
‘Thank you, doctor. I would like you to do it. I don't want to watch. I just want to know it's been done.’
‘I'll go and do it now. I'll come back in a few minutes.’
I left her and fetched one of the ward ‘cut down’ sets. These were small silver boxes with the necessary equipment inside to enable you to make a cut through the skin and dissect out a vein when you could not find one to put a cannula into directly from the outside. There would be a scalpel inside that would do for the job. I took the box to the end of the ward where Mr Jones was still lying in his bed soon to be laid out formally by the nurses. He looked so pale and quiet and peaceful compared to the living man who had been there just an hour earlier. I took the cold wrist in my hand and with the scalpel from the silver box I made a small cut where I knew the radial artery would be. Yes, there it was. Even in death it was a distinct structure. I pressed the blade against it and firmly cut across it. Of course there was no bleeding for the circulation had ceased one hour ago at the moment of death and the blood had clotted soon afterwards. Later the clot had retracted and squeezed out the serum from the clot. That was why there was ‘shunting’, as it was called, within the eye vessels when you looked at them with an ophthalmoscope after death. Now I could tell Mrs Jones that truly her husband was dead. She could bury him in peace knowing that there had been no terrible mistake. There were some sutures in the cut-down set and I closed the small incision with a single stitch.
The rest of the morning was spent in the wards sorting out, as best I could, problems that had arisen overnight. This varicose ulcer was not healing well; could we change from acroflavine to Lotio Rubra[2]? This lady's wound was looking infected; could we take the stitches out? This man's intravenous infusion had tissued; would the doctor, please, put up another one? When I looked at the patient's arm my heart sank because there did not seem to be a vein anywhere at all, just a lot of bruises? Then I remembered what one of the anaesthetists had told me about putting the arm in hot water to make the veins stand out. This particular arm was rather puffy with oedema fluid but I had learnt also that if I took the warmed arm out of the basin and dried it quickly so that it did not get cold as the water evaporated I could squeeze it and the oedema fluid would disappear temporarily. There was then perhaps a couple of minutes, but probably less, in which to pop the cannula into one of the veins that you could now see. To my relief it worked like magic! The metal cannula was horribly blunt (why didn't they sharpen them more often?) but by pushing hard through the bleb of local anaesthetic that I had injected just below the skin I had managed it. What a relief!
During the afternoon I was asked by the casualty officer to admit a man with an ischiorectal abscess. I went down to Front Surgery to see for myself. The abscess was enormous. It would have to be incised. As the old adage said: ‘never let the sun go down on undrained pus!’. Unfortunately the patient had eaten a big lunch despite his painful backside, so I arranged with the theatre sister that it could be done sometime during the evening. Having fixed this up I contacted the resident anaesthetist on call who said OK, and that was that!
Then my combination of lights came up again. I rang the porter's lodge. Would I go to Lydia ward, please, as quickly as I could, as a patient had collapsed. I ran up the stairs. When I got to the ward I found it was the old man who owned the barrow who had suddenly gone pale and unconscious. The nurses had given him oxygen by a B.L.B. mask[3], had lifted his legs up in the air and had injected both Methedrine and Coramine[4] intramuscularly into his thigh. Whether it was due to this treatment or not, the old man had promptly woken up, and was now demanding that he be left in peace. I examined him carefully but he seemed to be all right.
‘You must have fainted, Mr Bennett, but you're OK now.’
I turned to the nurse. ‘He had better go onto a quarter hourly pulse and blood pressure chart for the next hour or so, but he seems to have recovered from whatever it was. Thank heaven for that, I thought to myself. I would never have been brave enough to open his chest[5] and massage his heart. Still I would not really have been expected to do that with an old man like Mr Bennett, but in a younger patient I would have had to do it. There was a scalpel in a box on the wall in each ward so that time would not wasted in an emergency.
It was fairly quiet from then on till supper in the mess. At supper the new housemen were swapping tales of how their first day had gone, and also asking for advice about problem patients from the old hands, last year's housemen who were now ‘third house-job’ men, or even senior house officers. There was a moment of male hilarity when someone shouted down the table to one of the girls ‘have you got the mustard up your end, Elena?’. Then Dick made the mistake of saying that he had forgotten to give one of the patients who had been discharged back to the local doss-house the antacids he should be taking for his ulcer. The ‘old hands’ went on and on about how terrible it was and what would happen if the ulcer perforated till Dick could stand it no longer. To everyone else's intense amusement he ended up at ten o'clock at night borrowing one of the midwives bikes and cycling down Tooley St to the doss-house with the Nulacin tablets in his pocket.
After supper I phoned Isabel to tell her about the day so far, carefully not mentioning my many anxieties, and then it was time for my ‘night round’. Tradition required me to visit every ward where I had any patients, and to sit down formally with the staff nurse to go through the observation charts of the patients and discuss any problems that had arisen.
I climbed the stairs to Samaritan ward and rather nervously opened the door. My first night round was about to begin! The day had already been one huge culture shock for me; would this be another? I introduced myself to the staff nurse on duty who said she was very busy, could I possibly come back in half an hour when she would have finished giving out night sedations. I retired feeling rebuffed yet fully appreciating that the nurse had more to do than I did at that moment. I had lost the first battle but not the war!
Somewhat discouraged I went and sat on a bench in the park, as the central area of the hospital was affectionately called. The summer's evening was mild with a gentle refreshing breeze. I found it peaceful and relaxing, and I was joined by one of the resident pathologists who used to boast (quite untruthfully) that he never cross matched any of the blood needed for transfusion, he just added ten milligrams of Piriton (an antihistamine drug) to each bottle. By the time the half hour was past my spirits were high and my mood confident once more. I went back to the ward where the nurse made me welcome this time. We sat together at the table in the middle of the ward where the observation charts were all ready in a neat pile. She picked up the top one and passed it across to me.
‘Mrs Drake had a hernia repaired two days ago. Her temperature is slightly up to-night, but otherwise she is well.’
I looked at the chart. Yes, her temperature was 99.6o F and her pulse was 100. She must have an infection somewhere. The surgical incision, her lungs, or perhaps her urine.
‘I'll have a look at her when we've finished looking at the charts.’
‘You'll be busy then. They all have temperatures to-night.’
She was right. All five of my patients in the ward who had had their operations in the previous two days had mild fevers above 99o F. I insisted on listening to their chests. All clear. Pain when passing water? No. Pain or tenderness in their incision? No. Tenderness in their calves? No. Sorry to have woken you up. See how you are in the morning. Wonder what on earth was wrong with them. Baffled and unsure I left the ward. Luckily the other wards produced no problems. Now it was time to see what time my patient would be going to theatre to have his abscess incised.
I phoned the theatre sister and was told that at last the time for my patient to go to theatre had arrived. The duty surgical registrar was on his way and the anaesthetist was just about to start the anaesthetic. I ran up the stairs. I was not going to miss seeing my first emergency admission having his operation.
The anaesthetist injected some thiopentone into a vein at the patient's elbow. He settled him on some Trilene for several minutes and then turned on the ether. I watched the gases bubbling through the clear sparkling liquid and marvelled at the wonder of anaesthesia. It took a full eight minutes to get him down to stage three, with much coughing and spluttering and breath-holding on the way. At last they put his legs up into the stirrups and the surgical registrar stuck a scalpel blade into the abscess. A stream of thick creamy pus poured out. Even the ether could not entirely hide the foul smell. Probably E. coli, I thought. I watched as a second cut was made at right angles to the first one, so that now the roof of the abscess had been incised in the shape of a cross.
‘I'll have some hydrogen peroxide, please, nurse, to wash out the cavity, and then a Eusol[6] pack. Thank you.’
Soon the job was done and the patient on his way back to the ward still sound asleep. The nurse who came to collect him had the post-anaesthetic tray in her hand with its mouth-gag, its boxwood wedge and its tongue forceps in case he should vomit or obstruct his airway. Back on the ward they would put him somewhere near the nursing station with the light on so that they could keep an eye on him until he woke up.
Good Heavens, it was one o'clock. Time to go to bed. I climbed the stone staircase to the third floor. I was tired. Would anybody need me up during the night? I knew the porter would come and wake me if they did. Let's hope not.
I fell asleep with the lingering smell of ether still in my nostrils.
Guy's Hospital
I finished my time as a houseman feeling quite unprepared for general practice. It seemed amazing to me that I could now go out into the wide world as inexperienced as I was and put up my plate. Certainly I was not ready yet for that.
So I looked each week at the jobs vacant columns in the British Medical Journal, not really knowing what I was looking for. I had always remembered my time doing anaesthetics as one of the very best of my student appointments. There was so much standing around as a student, not actually doing anything useful, that it had been a real delight to be able to put up ‘drips’ and do a few practical things. It made you feel that you could actually help look after people.
I remembered the first time I had put an endotracheal tube down a patient's windpipe. It had seemed an enormous achievement, and in a way it had been. I relived the moment: first I had picked up the laryngoscope and put it the blade carefully into the patient's mouth, slightly on the right side. Then I had moved the handle forward a short way so that the blade moved forward too, pushing the tongue to the left. Now there was an open space that I could look into, past the uvula to the back of the throat. Then I had let the blade slide deeper keeping it close to the back of the tongue. Soon the epiglottis, the curved cartilage guarding the entrance of the larynx, had come into view. I had let the tip of the blade come to rest just where the tongue and the epiglottis met and had lifted the handle upwards towards the ceiling, and a little forwards, so that the tongue and the epiglottis had been lifted too and the vocal cords were exposed. Then I had picked up the endotracheal tube and had guided it through the cords into the trachea. What exhilarating fun!
So when I saw the advertisement for a Senior House Officer in Anaesthetics at Taunton, in Somerset, I thought long and hard. Was this the job for me? Well, it might be, but I wasn't sure. I certainly wasn't ready for general practice and I was really rather overwhelmed by the many possible ways my career could go. I didn't see myself as a surgeon - too much like a prima donna for my liking, and anyway the career ladder was far too daunting. ‘General Medicine’ was very clever no doubt, but somehow rather unworldly and unlikely. It was difficult to believe in many of the diseases you were taught about, even though you had seen them in the wards. Bleeding from a duodenal ulcer was one thing - after all that had happened to mother - but how could you really believe in disseminated lupus erythematosis or brucellosis? It was rather like believing that people really did understand French and enjoy ballroom dancing.
I phoned the hospital administrator at Taunton.
‘I wondered if the SHO post in anaesthetics was still free.’
‘Yes, it is. Let me get the consultant who is dealing with it to speak to you.’
I waited a few moments and then a new voice:
‘From Guy's you did you say? When would you be able to start?’
‘I could start on September 1st, but I would like to know a few details about the post. Could you send me the job description, please?’
‘Yes, of course. Are you sure you could not start sooner than September?’
‘No, I am sorry that's the earliest I can manage.’
‘Never mind. It will do splendidly. Ring me in a couple of days and we will have everything fixed up for you.’
I came off the phone in a state of high elation. I was very surprised that they had not already filled the post, but then I was naive and inexperienced; I had no idea what a chronic problem it was in Taunton as far as getting junior staff was concerned.
Later, after a letter and few more phone calls, I began to realise that I had the whip hand in the situation, and finally I said that I would take the job only if they would let me live out when I was on call. That they agreed to have a nonresident ‘Resident Anaesthetist’ shows just how desperate they were.
We found a nice flat on the third floor of a house opposite a bowling green, a few minutes drive from the hospital once the busy daytime traffic had died down. The landlady was a kind gentle soul whose sister owned a cider factory down the road in Norton Fitzwarren. The rent of £4-10-0d a week for the flat included a regular flagon or two of the golden nectar. No wonder that I developed a liking for the stuff!
The resident medical staff at the hospital were a particularly fine bunch of young people from all over the world. The one Englishman amongst them was known affectionately as Dr. Livingstone. Some evenings Isabel and I ate in the mess because Drs Rasti and Singh made such wonderful curries.
On my first day at work Dr Pitts, one of the consultants, showed me how to anaesthetise the children who were to have their tonsils out. It was very similar to the way that I had watched being used at Guy's, but it was so much more exciting now I was actually about to have a go myself.
Over the next few weeks I got really quite skilled at persuading the small children to breathe the ethyl chloride that I sprayed onto the Schimmelbusch mask, and at judging the right moment to change over to ether, and when to move from the anaesthetic room into the theatre and let the surgeon pop in the blade of the Boyle-Davis gag in the child's mouth so that we could connect the black rubber tubing from the anaesthetic machine to the bulbous end of the metal tube which was welded onto the blade of the gag. Then we would let a steady stream of gas-oxygen-ether flow down the metal tube so that finally it came out of the other end deep in the throat just above the larynx. It was tremendous fun, but Isabel used to complain when I got home.
‘John, I can smell the ether on you for days after you do a tonsil list. Are you sure you are not getting too much of it to breathe yourself?’
A very perceptive question indeed, but I dismissed it without giving it even a moment's consideration.
‘You worry too much dear. But all the same I'm sorry if I stink of the stuff. It's very difficult to keep away from it when you are pouring it all over a Schimmelbusch mask. Is it very unpleasant?’
‘Oh, it’s not too bad, but I do think you should try not to breathe too much of it[1].
‘Yes, dear.’
I was not to know at the time that she was seventeen years ahead of the rest of the world.
Catterick, Yorkshire
It was a cold sunny day as I motored up the A1. The countryside in North Yorkshire was so green and pleasant, despite it being January, that I wondered if somehow I had lost my way. Surely Yorkshire was all black industry, coal mines and slag heaps; that at least was the picture I had been expecting, never having travelled north of Shrewsbury before this day. I was feeling nervous about my sudden posting and was worrying about Isabel as well. They had only let her out of hospital early after her appendicectomy because I would be there to look after her, yet here I was posted at two days notice to Catterick. The rumour was that the regular anaesthetist there had been found in a linen cupboard with one of the nurses and had been posted overseas in a hurry. I had no idea if this was true or not. Anyway I had had to leave Isabel behind to cope somehow. Tim was nearly nineteen months old now and he was certainly a handful. I hoped they both would be all right. I laughed as I remembered just how anxious Isabel had been before her operation. She had said to Frank:
‘I'm not frightened of the operation, it's the anaesthetic that worries me. You will make absolutely sure that I'm properly asleep before you paralyse my muscles with those drugs you use, won't you?’
‘Yes, of course I will. You will be fine,’ Frank had replied, and, of course, she had been!
Here at last was the turning to Catterick. I swung the car off the A1 and, passing the race course on my left, I came a mile or so later to the famous (or was it infamous?) camp where my father had been for a short while in the first world war. It looked rather bleak in the fading light. I followed the signpost to the hospital and rather nervously asked a soldier the way to the RAMC officers mess. It was quite an adventure really.
Later I phoned Isabel to tell her that I had arrived safely. She was tired but OK. Tim was asleep and she was planning an early night herself.
‘I'll phone you to-morrow, my darling. Keep your spirits up. I love you very much.’
‘And I love you too. Have you contacted Peter yet?’
‘No, but I'll do it now.’
Peter was the other anaesthetist at Catterick (the one who had not been posted away at short notice!). He and I had been at Cambridge together. Ivor and I had shared a bench next to Peter and Tim in the biochemistry lab. Peter was a quiet gentle fellow with a silver streak in his hair. I phoned him up to say I had arrived and I was immediately asked round for supper.
‘We have got an ENT list to-morrow afternoon,’ said Peter in his soft gentle voice. ‘Mostly children, I think, but there probably going to be a couple of soldiers at the end.’
‘That will be fun,’ I said, ‘I haven't done an ENT list since leaving Taunton. I'll enjoy smelling the old ethyl chloride and ether once more.’
‘Ethyl chloride and ether, eh? Here we usually give the kids gas, oxygen and halothane, or sometimes thiopentone, followed by sux and a tube.’
‘You intubate the children, do you? I've not seen that before for tonsillectomy except in adults,’ I said. ‘We always did the children without a tube at Taunton. You know, insufflating ether down the sidearm on the tongue plate of the Boyle-Davis gag. I'll be interested to see it done with a tube.’
It worked very well. The first child arrived in the anaesthetic room fast asleep on his Vallergan premed. I watched as Peter carefully let some nitrous oxide, oxygen and halothane flow across the child's nostrils. After a minute or so he lowered the mask gently onto its face and I injected some scoline intravenously. Then he took the red rubber endotracheal tube and slipped it between the child's vocal cords. The connector on the tube was placed in the opposite direction to usual. It was specially designed so that the tongue plate could not squash it and thereby obstruct it, which would be disastrous. The tongue plate itself had a slit along its length so that the tube fitted into it and was not squashed either. It was called the ‘Doughty’ modification after the doctor who had designed it[1]. The afternoon proceeded without any problems and I was most impressed with the technique. Why, I wondered, had they not done it this way in Taunton? Well, their method had stood the test of time, so that was probably reason enough. Still this did seem to be an improvement. It had all been most interesting.
When I got back to my room I could not resist looking in my much thumbed copy of Synopsis of Anaesthesia. I read:
For tonsil dissection, an endotracheal tube is preferred by many; objected to by some. It can be passed through either the nose or the mouth. Ethyl chloride is given until about ten stertorous breaths have been taken, then a lubricated Portex tube of suitable curvature (obtained by boiling it on a curved stylet) is passed blindly from the nose into the trachea.... If the patient regains his reflexes before the tube finds the glottis, more ethyl chloride can be given and a further attempt made at intubation. The deep breathing and relative insensitivity of the larynx produced by ethyl chloride make it a very suitable agent for intubation in children.’
Well fancy that! Despite all my experience with ethyl chloride I had never seen that done. Now it looked as though I never would. The technique Peter had showed me this afternoon really did seem an improvement on the old way, and now I had seen it I would certainly adopt it.
It came as something of a surprise, therefore, when later that week I found that the civilian ENT surgeon who came across twice a month to Catterick from Darlington did not like his tonsillectomies intubated, and he was pleased when I said OK I would do it the old way if he wanted me to.
The surgeon told me that he did a lot of guillotine tonsillectomies at Darlington under ‘a quick whiff of ethyl chloride’.
‘It's so much quicker. I can do ten cases in an hour if it goes well. That way I keep the waiting list short. Oh, it's true that about a quarter of them have to come back eventually to be done again. I do a proper dissection at the second go. If I tried to do that on all of the children my waiting list in Darlington would be years long, not just a few months. Yes, guillotine tonsillectomy is quick, simple and quite effective in a lot of cases.’
‘I'd like to see you do some,’ I said. ‘Would it be all right if I came over to Darlington some day?’
‘Certainly.’
As it happened it was nearly the end of the year before I managed to get there. I arrived at nine o'clock to find that the surgeon had completely forgotten that I was coming and, also, that the regular anaesthetist for the list had been held up dealing with an emergency elsewhere in the hospital. The surgeon had just got on with the work and acting as his own anaesthetist had already completed four operations single-handed. This was not so difficult really as I soon discovered.
The anaesthetist arrived at last and soon the production line was going even quicker. The anaesthetist was very skilful with the ethyl chloride. Within one minute of starting the child was in deep surgical anaesthesia. The administration of ethyl chloride was stopped, the gag put in the mouth and the tonsils whipped out one at a time. The child was turned onto its side over a pillow so that he was slightly head down and the adenoids were curetted; the slight head down tilt was maintained so that any blood in the throat would run out of the corner of the mouth. Within another half minute the child was crying and spitting bloody saliva into a bowl before being carried out of the room.
I timed the event carefully. With the small children it took just six minutes from the start of one case till the start of the next including the cleaning up in between. Clearly they were real experts. Some of the older children, those over five, were given a little ether after the ethyl chloride and this made the induction about a minute longer. The tenth operation of the day was completed before a quarter to ten.
Almost immediately the surgeon disappeared off to his outpatient clinic. I stayed a few minutes chatting to the civilian anaesthetist before leaving myself. The smell of the anaesthetic vapours was so strong that I was quite glad to get out of the room, out of hospital and into the cold crisp air outside.
Catterick, Yorkshire
‘I'm off to the library, Derek.’
‘OK, John, see you this afternoon.’
The library at the Military Hospital was a splendid place to work for an exam because it was warm, but not too warm, and it was never crowded except just before lunch. There were plenty of journals though not a great selection of books. Still that was not important as I had my own two anaesthetic ‘bibles’ - Synopsis of Anaesthesia, 4th edition, by J.Alfred Lee and General Anaesthesia by Wylie and Churchill-Davidson. I had bought my Synopsis when I had been Senior House Officer at Taunton and I had read it so many times that it had become like an old friend. True the yellow ochre covers were soiled and scuffed but the binding was sound and the contents fascinating and I enjoyed the telegrammatic style. Inside the front cover there were some appropriate aphorisms:
Eternal vigilance is the price of safety.
Relief of pain is purchased always at a price. The price in both morbidity and mortality does not greatly differ whatever the agent or agents used. (R.M.Waters)
The duty of the anaesthetist towards his patient is to take care.
While the anaesthetist's chief duty is to prevent and alleviate pain, his primary responsibility is to maintain respiration.
Primum non nocere - First of all do no harm.
All good stuff, certainly, but I had added a couple of my own near the bottom if the page:
Industry is the root of all ugliness. (Oscar Wilde)
Examinations are formidable even to the best prepared, as the greatest fool may ask more than the wisest man can answer. (Charles Caleb Colton)
When I reached the library I found Dick there reading up on computers.
‘I'm after this job with the Medical Research Council, you know. I'll be working with the anaesthetic research department at Leeds University if I get it. It'll be tremendously exciting. I'm not looking for any old job when I get back to civvy street. I want something that's out front.’
I found myself quite infected by Dick's enthusiasm. Good for him that he knew what he was looking for, and good luck to him in his attempts to get it. I didn't know anything about computers but it sounded fun enough if you did. It made a straightforward career in anaesthesia, like the one I was planning, seem very pedestrian. Still that was the way it was and that was the way it would be.
In the meantime here I was studying for the final examination to make me a Fellow in the Faculty of Anaesthetists of the Royal College of Surgeons of England and it was just two months away. I opened the book and started to read.
After half an hour of studying the various different anaesthetic circuits I found my attention wandering. I put the book down and picked up the bound copies of the monthly journal Anaesthesia for the year 1956. I turned the pages glancing at the titles of the articles inside.
Hypothermia for Neurosurgical Operations
Anaesthesia for Children and The Newborn
Trichloroethylene in Dental Anaesthesia
I must read all these sometime, I thought, but not just at this minute. I continued to flip the pages and came across some adverts:
A new OXIMETER for the continuous measurement of arterial oxygen saturation through the medium of the intact ear.
There was a picture of the device clipped onto an ear and also a box with dials on it for reading out the answer. Really clever!
Below this, in another advert, I read
BLEASE of LONDON
INTRODUCES the 'PULMOFLATOR'
modified for the treatment of
and there was a photograph of a machine for giving artificial respiration to people. I thought that it must originally have been designed for use during anaesthesia in lung and heart surgery, but I remembered that in 1952 there had been the most terrible epidemic of polio in Copenhagen. They had treated the patients with tracheostomy and hand-powered artificial ventilation using relays of students from the university. At one time there had been seventy patients being treated at one time in this way. Unlike the ‘iron lung’, which sucked the chest wall outwards from the outside, they had squeezed breathing bags borrowed from anaesthetic machines, forcing air into the trachea and so blowing the lungs up from the inside. Now it seemed that they had adapted anaesthetic ventilators to do the job, which seemed a very good idea.
I turned over more pages, skipping quickly onwards through the book.
That was curious, I thought, what could that be about? I read on:
Ethyl chloride, which has a boiling point of 12o C would not exist as a liquid at operating room temperatures unless it were subjected to pressure as in the 100ml sealed containers. At theatre temperatures this pressure is about 30-40 mm of mercury, which is sufficient to operate a rotameter.
Well, fancy that? Was there really enough pressure inside the seemingly frail glass bottle to work the flowmeter on the anaesthetic machine? It hardly seemed possible. I would never have thought that the glass was strong enough.
For the purpose of administration of approximately 300 anaesthetics the cyclopropane rotameter was used as there is no reducing valve between the cyclopropane yoke and the fine adjustment valve. The scale readings have to be corrected because for a given scale reading much less ethyl chloride flows than does cyclopropane.
It sounded great fun. Fancy having the idea of turning the glass container upside down and using the ethyl chloride as a gas through the anaesthetic machine. Brilliant! I wished that I had thought of it. Perhaps I should try it out?
The next day I looked closely at the machine to see how I could fit a tube from the nozzle of an ethyl chloride bottle to the bottom of the cyclopropane flowmeter. It looked easy enough at first glance, but when I tried to put it into practice it was a different story. I got various bits of rubber tubing and a few pieces of plastic tubing. Eventually I got it fixed up so that I could direct the ethyl chloride gas up the flowmeter, but in the end I felt it was too unreliable to try out on a patient. Still it had been a good idea.
Now that I had passed the final FFA exam it was nice to be able to go to the library for a reason other than swotting. As the winter months faded and spring was upon us once more, I would often browse through the journals and, in particular, look at the jobs advertised in the Lancet and the BMJ. It was a curious thing that a job might not seem very appealing when you read about it in one of these two journals, and yet the same post could sound quite attractive when you read about it in the other. I tried to analyse why this should be, but I never really got to the root of it. Often the wording was almost identical. It had to be something to do with the different print layouts, but I wasn't sure exactly what it was. As far as jobs were concerned I had always felt that when my national service was over I needed first to get back to a teaching hospital at registrar level, to get my foot in the door again so to speak, but hoping at the same time that I would not have to wait too long before a senior registrar post came up. It had been quite a shock to me when I had visited the anaesthetic department in Newcastle to discuss my future. To my amazement the professor there had wanted me to take one of the consultant posts in the region that they could not fill. It seemed that there were several of these in the north east of England and as he pointed out I had both my FFA and would have nearly five years experience in anaesthesia when it was time for me to return to civilian life.
‘I don't understand you young men of to-day. Why not take one of these posts, in Middlesborough or wherever, and do it for five years as a consultant. You can always move on then if you want to. I don't see why you need to be a registrar at all, when I've got consultant posts I can't fill.’
Well, it was certainly a new way of looking at my future. I knew that it was unlikely that I would take him up on his offer, but I promised to give it some thought. It was more likely that I would try to get to Bristol, as both Peter and Derek had done when they had left Catterick, and anyway that seemed the logical move for someone who had started his anaesthetic career in Taunton. I would have to see what Isabel thought about it. Anyway, there didn't seem to be any registrar posts coming up in Newcastle for a month or two. However, there was a job advertised for a senior registrar in Aberdeen, and I did write off for details and an application form; after all if the man in Newcastle wanted me to be a consultant then perhaps the man in Aberdeen would at least agree to me being a senior registrar.
I heard nothing from Aberdeen for eight weeks, so I phoned the Regional Health Authority. A plummy voice told me that the job had been filled. I demanded to know why no-one had written and was told that they did not have time to write to every unsuccessful candidate. I was incensed, and said so, but I failed to get any apology of any sort. So I phoned the head of the anaesthetic department in Aberdeen.
‘I’m afraid it is nothing to do with me,’ he said.
‘That’s not true,’ I retorted. ‘It is the business of everyone in Aberdeen, and especially the person at the top, if people are behaving like this when they are acting for them. I think you should contact them, and complain bitterly, and see that nothing like this ever happens again.’
He said he would, and apologised on behalf of the people at Region. I never did hear from them.
Then there was a registrar job at Cardiff. They did not give me the job but at least they gave me an interview. The professor spoke to me afterwards.
‘I am sorry we did not give you the job, but I think you badly need a job like this one, to get you back onto the civilian ladder.’
‘That’s exactly why I applied for it,’ I said grimly, wondering what the young SHO from Frenchay Hospital had got that I had not got; a reference from an old friend of the professor, I guessed. I discovered later that this was exactly the case, but I hold no grudge. Though, clearly, it was who you knew, not what you knew, that mattered.
So I contacted Derek, who had gone to Bristol when he had left Catterick. He arranged for me to visit Fen, who was the consultant in charge of the NHS department at the Royal Infirmary, and when I was there I also met up with Peter, who had been at Cambridge with me, though he had been in a different college. He had not had to do National Service and was now a senior registrar. He had, till recently, been the only anaesthetic SR in the whole of the SW region. Now the establishment had been increased from one to three, and Derek had been promoted to SR, as had Alan, whom Isabel and I had known at Guy’s. This meant that there were two registrar posts about to be advertised. A good time to come! Peter introduced me to Fen and pointed out that they really needed at least one locum registrar, if not two, until such time as the definitive appointments were made. I left at the end of the afternoon with a locum post starting the following Monday, and an application form for one of the two substantive posts. As Fen put it:
‘Peter, if I came into your shop for a bicycle, you would sell me a bus!’
Clearly having the right friends can be very useful, as I already knew.
Bristol was bang up to date in many ways and yet old-fashioned at the same time. At the Children's Hospital many of the tonsillectomies were still done with nitrous oxide, oxygen and ether insufflated down the side tube of the Boyle Davis gag tongue plate while guillotine operations, usually under ‘a quick whiff’ of nitrous oxide and halothane (rather than ethyl chloride), were not uncommon. One ENT surgeon, a brilliant operator and fine clinician, truly believed that there were no cases of his that ever had to go back to theatre because of bleeding after guillotine tonsillectomy when in reality there were one or two every six months; the junior surgeons would routinely re-operate to tie off the bleeding vessel without telling the boss about it. Such is the way that myths in medicine arise!
It was strange for me to return to the old way of doing things for by this time at Catterick they had gone over totally to anaesthetising for tonsillectomy in children with the help of an endotracheal tube. Luckily using ether was like riding a bicycle - you never forgot how to do it!
One afternoon, shortly after I had arrived in Bristol, I was working with one of the consultant anaesthetists, a short portly and pompous man with a large private practice, which often seemed to clash with his health service commitments. We were doing a tonsil list , and in due course we got around to discussing how one should re-anaesthetise a child for postoperative bleeding after tonsillectomy.
‘There was an interesting paper[1] in the BJA earlier this year by a man called Denison Davis,’ I said. ‘He thought that the best thing to do was first to crossmatch some blood and restore the blood volume, then to empty the stomach, if possible, and to clear all the clots out of the pharynx and postnasal space before anaesthetising the child with 4% halothane and 96% oxygen, and when they were deep enough to pop a tube through their cords.’
‘I don't agree with that. Nitrous oxide and oxygen and a little ether is all that is ever required, and I have never found it necessary to intubate the trachea, and you should not use ethyl chloride or relaxants, as they may be dangerous; 4% halothane sounds to me to be as bad as ethyl chloride, as it drops the blood pressure dramatically, especially if there has been a lot of blood lost. As it happens I, too, have just written a paper[2] on the subject. It should be in the October issue of Anaesthesia; at least, that's what they said the last time they wrote to me. However, I do agree that it is essential to give some blood or plasma, and to remove any clots in the nose or pharynx before you start. I always look round the throat with a laryngoscope while the child is still awake, though it isn't usually possible to put a stomach tube down until later and I often wait till after the surgeon has controlled the bleeding before I do that.’
‘But wouldn’t it be safer with a tube?’ I asked, thinking of all the blood swilling around the throat at induction of anaesthesia. Certainly since Peter had shown me how satisfactory it was with a tube, I had always assumed that it was the best way of handling a ‘bleeding tonsil’.
‘No,’ he replied. ‘It is much easier to use posture, gravity and suction to keep the blood away from the larynx than to fiddle about trying to put a tube down. I have done about eight cases a year for the last thirty five years, so I ought to know what’s best. Keep things simple and you will keep yourself out of trouble.’
I decided both not to argue the point and to continue using an endotracheal tube for these cases.
That afternoon I had time to go to the library and look out the Denison Davies paper again, and read it more fully, as I had actually only read the summary and glanced at the paper previously. It was amazing how badly I had misquoted it. I had remembered correctly the 4% halothane for induction, but I read now that he often maintained anaesthesia with ether, given with oxygen down the side tube of the gag tongue-plate, and he too did not intubate children, but relied also on posture, gravity and suction. It did not alter my decision to continue intubating ‘bleeding tonsils’ when I met them, but I made a firm resolve not to quote articles in future unless I had read them properly.
Denver, Colorado
I really enjoyed myself at the hospital in Denver. The staff were a most amiable bunch of people, including Vi, the nurse anaesthetist who told me that she had taught the professor when he had been a student. She had a wonderful fund of stories of the old days.
‘Why, John,’ she said to me one day, ‘I guess we did some pretty strange things. I once used a Schimmelbusch mask to give ether for a posterior fossa exploration in the prone position. I started out with the patient on his back, and took him deep enough to put a tube down. Then we rolled him over and I had to sit under the operating table dripping ether onto the mask before I held it up to the patient’s face with the tube sticking out of his mouth.’
‘That’s amazing. Did it work all right? ‘
‘Oh, it worked splendidly, but I had to keep on putting my head out from under the towels so that I did not put myself to sleep. We don’t use much ether these days and when we do we use the copper kettle. It is not so much fun as it was!’
Now, after a wonderful year, it was time to leave Denver. I had got hold of some splendid containers in which packs of dialysis fluid had been delivered to the hospital. These were the size of tea chests but circular. They proved grand things for packing up all the clobber we had acquired over the year, including the Corning heatproof glass dishes which Isabel had bought and the artificial Christmas tree. We had thought long and hard about whether to stay in the USA, but even the temptation of $60,000 a year to work in Cody, Wyoming, had not been enough to persuade us.
‘I know it's a lot of money, John,’ Isabel had said, ‘but we might just find ourselves on the Ho Chi Minh trail if we stay.’
‘We'd probably would be all right, you know, as I've already served with a NATO force, but I do see what you mean. We would feel pretty stupid if we stayed for the money and ended up fighting their war for them.’
‘Anyway, I want to go home first and see what happens. Let's give it a couple of years. If we are not firmly settled by then we'll think about coming back here.
‘OK dear, that's what we will do then,’ I replied cheerfully, but at the same time thinking to myself how strange it was that I should be going home so readily to a third of the salary I was getting in Denver and a twelfth of the salary that was on offer in Cody. Still money wasn’t everything, was it?
My last day at work was something of a dream. I arrived at the hospital to find a green gown had been made for me to wear over my theatre garb with ‘King for A Day’ in large letters on it. All morning everyone made a big fuss of me and at lunchtime they took me off to the Happy Tavern to drink my health, and wish me good luck and farewell. I was totally surprised by it all and considerably moved as well.
Back in the apartment block in Cherry St there were other goodbyes to be said and the neighbours gave Isabel and me a plate with the family crest and name on it which still hangs on our dining room wall to-day.
Early the following morning we flew to New York where we spent an wonderful day. Kennedy airport with its bustle and its symmetry was quite fascinating, and then there was the helicopter trip to Manhattan. I took a photo of the Empire State Building as we passed by, the tall skyscraper appearing obliquely in the window as the plane banked. I was about to take a second picture when Isabel cried out
‘John, John, we are dropping like a stone. I think we are going to hit that building.’
I laughed. I had forgotten to tell her that the heliport was on the roof of the fifty six storey Pan Am building! When she climbed out of the plane she was shaking visibly but she soon pulled herself together. She was very excited when she discovered that Grand Central Station was at the bottom of the building.
‘I've always wanted to see Grand Central Station,’ she cried out. ‘People in books are always meeting under the clock at this station. What fun!’
During the morning we took the lift to the top of the Empire State Building and gazed with awe at Central Park and the great skyscraper city laid out before them. After a hamburger lunch we took a taxi to the Staten Island ferry and excitedly steamed past the Statue of Liberty. Looking at the skyline of Manhattan from the ferry was a memorable moment in an altogether fascinating day in an (but exhausting) city.
At six o'clock we were back at Kennedy airport.
‘It's amazing,’ Isabel said. ‘All these people waiting so casually for a plane to another city. If you didn't know you'd think they were just queueing for the bus.’
Soon we were in the air again on our way to Boston; in less than thirty minutes we were back on the ground where Ivor and Mary and their four children were waiting to meet us. Mary was thin as ever, looking as though she needed a good square meal, as did the children too. Though he made them welcome enough Ivor was clearly preoccupied. He explained that he had been working in Boston for six weeks now and he had just discovered that the hospital authorities did not automatically insure him against malpractice claims and that in any case his licence to practice medicine was not valid in Massachusetts. All this in the state where six months earlier an anaesthetist had had half a million dollars damages awarded against him after a mishap. No wonder he was worried!
‘It's not my fault really,’ he said. ‘After all, the hospitals in Seattle and Charlottesville saw to all that for me. I didn't have to make any of the arrangements myself. How was I to know that it was all different here?’
How, indeed? But how like Ivor not to check! Still it was great to see them all again, and to sit late talking of old times.
Next day Mary and Isabel took the children out while I went to the Massachusetts General Hospital. I was keenly looking forward to seeing the very room in which William Morton had given the first successful demonstration of ether anaesthesia. On the way I visited the department of anesthesiology and met an old friend, another John, who had been at Cambridge with me but who had come to the USA at the start of his career and become very well known on the American anaesthetic scene. I had read several of the papers that he had been involved with.
The old operating theatre had been preserved as a memorial to that day, October 16th 1846, when Gilbert Abbot had breathed ether from Morton's glass inhaler and the surgeon Charles Warren had removed a vascular tumour from his jaw and had uttered those special words ‘Gentlemen, this is no humbug!’
When I got there I found the old theatre had all the sense of drama and of history that I had expected of it. The open space in the middle of the room was where the surgery had taken place, and round it wooden benches rose upwards in semicircular tiers so that the room looked like a miniature Roman amphitheatre. I tried to imagine the scene as it had been that day one hundred and twenty years previously. Where was Dr Morton? The surgeon, Charles Warren, was waiting impatiently. The patient, Gilbert Abbott, was pale and sweaty, his pulse racing with fear. Here was Morton now, just in time to hear Warren say
‘As Dr Morton has not arrived I presume he is otherwise engaged.’
Breathless apology and a request for time to assemble the apparatus ... Morton retiring outside for a few moments... the ether poured onto the sponge inside the glass globe... here is Morton back again.
‘Well, sir,’ said the surgeon, ‘your patient is ready.’
Reassurance from Morton to the patient. There on the front bench was Eben Frost, the man who had breathed the vapour on the evening of 30th September so that a tooth could be pulled without pain.
Morton offered the tube from the inhaler to Gilbert Abbott who took it and placed it in his mouth. He breathed the vapour for about four minutes.
‘Sir,’ said Morton, ‘your patient is ready.’
The hurried operation and the slow awakening several minutes later... no pain, ‘only a blunt thing scratching my cheek.’
Then those memorable words: ‘Gentlemen, this is no humbug.’
I stood quietly for a few minutes. I was strangely moved. I resolved to come back sometime in the years ahead to relive the moment once again.
That afternoon we walked through the campus at Harvard and then we took a taxi on a sight-seeing trip around Boston. There was not time to stop at the cemetery where Morton was buried, though I knew how the epitaph on his tombstone read:
William Thomas Green Morton, Inventor and Revealer of Inhalational Anesthesia: Before Whom, in All Time, Surgery was agony; By Whom, Pain in Surgery was Arrested and Annulled; Since Whom, Science has Control of Pain.
William Morton, from the Clendenning Library
A.D. 1968
Southmead Hospital, Bristol
I had been at Southmead a few weeks before I saw Terence using ether, which was interesting as by now it was rarely used, even for tonsillectomies, because of the increasing use of halothane (see chapter 6). One morning I went into his theatre to see if he would swap a night on call with me. He had the EMO apparatus out and was giving gas-oxygen-ether to his patient by a facemask placed over a nasal endotracheal tube with a safety pin stuck through it so that it would not disappear through the nostril into the nasopharynx.
He was explaining the machine it to the young registrar, who was with him for the morning. He was in grand form.
‘EMO, stands for Epstein-Macintosh-Oxford. Epstein was the physicist that Robert Macintosh employed to work in his research department at Oxford, and they have done a lot of good things between them, including the EMO. They designed it really as a draw-over vaporiser using ether-air, but it works just as well attached to a Boyle’s machine. Of course, on its own, or with the Oxford inflating bellows, it is very portable, and rugged; just the thing for anaesthesia in far away places difficult places, though, of course, there is not much wrong with ‘rag and bottle’ if you are up against.’
He turned to me. ‘What about Flagg’s can?’ he asked me. ‘Have you ever used that?’
‘No, I haven’t, but I bet you have.’
‘Of course. It works really well, you know.’
He turned back to the young registrar and explained that Flagg’s can was a tin can with several holes in the top with some ether in it which you connected to an endotracheal tube so that the patient breathed in air which had been sucked over the surface of the ether.
‘I like to use ether now and then,’ he continued. ‘Its such marvellous stuff. I can't understand why you young folk keep using muscle relaxants all the time. It's only 'paralyze and puff' or 'flick the Fluotec' these days. I ask you what's wrong with good old surgical anaesthesia, particularly with an agent like ether that keeps you breathing so well. Surgical anaesthesia is like marriage, you know - an honourable estate ordained by God.’
I laughed.
‘Perhaps you are right,’ I said. ‘But ether is still explosive, and on occasions there are some advantages to relaxing and ventilating a patient, or 'paralyzing and puffing', as you call it.’
‘Not many,’ he replied cheerfully; then, more forcefully, ‘I hear some anaesthetists are using long-acting relaxants for ENT operations. I think they must be mad. Fancy abolishing spontaneous respiration for an operation on the nose.’ And then changing the subject abruptly, ‘Did you hear about Billy and the nurse from Trinidad? He wanted to have the patient's arm out on an arm board, so he said to her 'arm board, nurse'. No response. So he repeated his request, 'arm board, nurse'. She replied: 'Ah'm bored, too, doctor'.’
I laughed again. I looked more closely at the set-up. The EMO had a solid, friendly and reliable look about it, and it did seem to be working very well, even if it was perched rather precariously on the table of the anaesthetic machine. The patient was taking regular deep breaths that contrasted favourably with the shallow rapid breathing you so often saw with halothane. Perhaps Terence did have a point.
‘I have used lots of ether in my time, but I have never known what concentration I was using. Once in Denver I saw ether put into a copper kettle, but I never mastered the arithmetic, so I still didn’t know what concentration they were using. What do you set it at on the EMO?’
‘Oh, I use up to 15% or so for induction, sometimes more, and about 6% for maintenance. In the long run you have to watch the patient. She'll tell you whether you are giving her too little or too much. Nobody really needs a calibrated vaporiser to give an anesthetic, do they?’
We were sitting in front of the fire reading quietly when the phone went.
‘I wonder who that can be?’ said Isabel. ‘I wasn't expecting anyone to ring to-night.’
I got up from my chair, slowly because it had been a busy day and I was tired, and walked towards the door. Sometimes I wished we did not keep the phone in the cloakroom under the stairs, but still it was convenient enough once you got there to be able to talk in peace without having to compete with other things going on in the room.
‘Hello.’
‘Hello. It's David here. I know you are not on call but we have a terrible problem in the intensive care unit. It's a sixteen year old girl with asthma. She arrived about an hour ago, blue, fighting for breath, moribund. She was given adrenaline, aminophylline, and steroids in casualty but she got worse and worse. We've intubated her but the bronchospasm is so bad that we can't ventilate her at all. We've tried everything we can think of. We've even given her ether but it hasn't helped. Now she's so bad that we can't get a blood pressure, or feel a pulse anywhere, and we can't ventilate her at all, though the ECG is still going and her pupils are still reacting at the moment. I'm sure she won't last long enough for you to get here. We just wondered if you had any last minute suggestions before she died.’
I felt the adrenaline surge through my body, my normally slow pulse racing ahead and leaving me almost breathless. There was sweat on my hands and the hairs on my arms were standing on end. Dear God, what was I meant to say to solve a problem like this from six miles away.
‘I'm coming in,’ I said, and I put the phone down. No sooner had done so than I realised there was one thing I should have reminded them to look for.
‘Isabel, I've got to go into the hospital as quickly as I can, but please do something for me. Phone the ITU and say are they quite sure the girl with asthma hasn't got a tension pneumothorax? Thanks.’ And I was gone.
The journey was a nightmare. I drove furiously but even as I did so I was acutely aware how important it was to arrive in one piece and not to kill anybody on the way. It wouldn't do any good to have an accident ? I might end up a patient in the ITU myself! Luckily the road surface was dry so that I could nip past slower cars without it being too dangerous. Still I was glad when I got there safely.
I screeched to a halt outside the door at the bottom of the slope where the ambulances brought the coronary patients. It was nine minutes precisely since I had put the phone down. I jumped out of the car, barking my shin on the edge of car door as I did so. I steadied myself for a brief moment, and then hurried through the door and down the corridor. I wondered whether the girl was still alive, or whether she was already dead as David had so gloomily predicted. I would know in a moment. When I entered the ward the tension in the air was almost tangible, and there was a strong smell of ether.
A small group of people were standing round the bed in the far corner of the room. David was at the head of the bed where he was trying to ventilate the girl by squeezing the black rubber breathing bag he was holding. I saw that Terence was with him, and so was the registrar of the medical firm under whose care she had been admitted.
‘She's still alive,’ said David, ‘but I can't feel a pulse anywhere and I can't get any oxygen into her. Look she as tight as a drum.’
He squeezed the bag to demonstrate how ineffective it was. She hasn't got a tension pneumothorax; we had already thought of that.’
‘Are you sure the tube isn't kinked or blocked in some way?'‘
‘Yes,’ said Terence, ‘we've changed it just to be sure, and the circuit as well.’
I looked down again at the girl, wondering what magical thing they were expecting of me. The young face was very pale but there was quite definitely still a pinkness in the lips. The tube through which they were trying to ventilate her was pulling at the corner of her mouth and I reached out and adjusted it. I looked at the her chest. The rib cage seemed quite out of proportion to the rest of her body... blown up like a balloon. There was the unmistakable smell of ether in the air. With all the electrical equipment about it was lucky that they hadn't blown the place up.
‘Let's try some more isoprenaline,’ I said. At least that was something to do while I was thinking what on earth I should be doing.
I laid my left hand on the top part of her chest just below the clavicle and struck the middle finger close to the nail with the tip of the middle finger of my other hand. It was just like tapping an empty box. Surely, I thought, this had to be a tension pneumothorax... the tympanitic percussion note, the distended barrel-shaped chest and the feeling of total obstruction to the flow of gas when the bag was squeezed. It must be.
‘Let me see the chest X-Ray,’ I said.
Someone held it up to the light so that I could look at it. They were right, of course. I could see the lung markings extending right out to the edge of the thorax. What a pity. If only it had been a tension pneumothorax we could have stuck a needle into it through the chest wall between the ribs and let the air out, so relieving the pressure. A dramatic and satisfying performance it would have been... but then they would never have phoned me up about something as straightforward as that, they would have calmly and effectively got on with it themselves.
Then suddenly, quite suddenly, I realised what was happening. Of course! There was air trapped inside the chest wall, and under considerable pressure too, but it was not outside the lung, it was inside it! I had seen this happen before, not in an asthmatic, but in a patient with chronic bronchitis. They must have blown air into the lungs and not allowed time enough for it to come out again. That would explain everything. The high pressure within the lungs was stopping the blood from getting through the lung capillaries. It would be having exactly the same effect on the circulation as a pneumothorax but instead of a collapsed lung it was an over distended one. No wonder that there was no blood pressure.
‘I think I know what has happened,’ I said. ‘I'm just going to disconnect the patient from the breathing circuit and see if we can let the lungs empty a bit so that some blood can get through.’
I pulled the catheter mount off the endotracheal tube, put a hand either side of the girl's ribcage and pressed firmly. I could hear a slow stream of air coming out of the end of the tube with a soft high pitched wheeze and some crackling bubbling sounds. Slowly, oh so slowly, my two hands started to come together. Fifteen seconds passed. No-one spoke. Another fifteen seconds and still the air came out and the hands got closer. Yet another fifteen seconds, and then one of the nurses cried out
‘I can feel a pulse at the wrist. It's quite strong. I'll see if I can get a blood pressure.’
A few moments later she said ‘it's 140 over 70.’
I breathed a sigh of relief. I reconnected the breathing circuit to the endotracheal tube and in a rather experimental manner began to ventilate the girl once more. One.. two.. three seconds to get a reasonable amount of air into her. One .. two.. three.. four.. five.. six.. seven.. eight.. nine.. ten.. eleven.. twelve seconds to get it put again. Three and twelve makes fifteen. Fifteen into sixty goes four times.
‘It looks as though we can only give her four breaths a minute if she isn't to blow up like a balloon again. We will just have to accept an enormously high carbon dioxide level but at least we will be able to keep her pink, and alive, that way. Let's try her on the machine.’
I pulled the Cape ventilator closer to the patient, connected her up to it and adjusted the controls.
‘Tidal volume 500 mls. Rate 4 per minute. There that's OK. Let's see how that goes.’
It seemed to be all right. I tried adding extra breaths but it was no good. So we left it at four a minute.
Shu arrived about this time. He was the senior registrar on duty and he had been busy for several hours with emergencies in the obstetric theatres. He offered to carry out bronchial lavage on the girl every 3 hours throughout the night, and in the course of this he produced some amazing inspissated sputum casts of the smaller bronchi, of which unfortunately we did not take photographs.
After eighteen hours there was some improvement and we were able to increase the ventilation to six breaths a minute, and then, later again, to eight a minute.
Four days later I took the tube out of her trachea, but she was not able to cope on her own. I had to put the tube back down and I arranged for the ENT surgeons to perform a tracheostomy.
After a further four days she was well enough to have the tracheostomy tube removed, and I wished then we had stayed with the nasal tube rather than do the tracheotomy. The following day she was well enough to go to an ordinary ward. A week later she was discharged home.
She was fine for four years and then suddenly, and quite unexpectedly, she died.
My bleep went off just as I sat down to lunch. The switchboard told me that the ITU wanted me to phone them. I dialled their number.
‘Could you come and see Mrs Cochrane, please. She seems to be swelling up.’
‘Swelling up? Which part of her is swelling up?’
‘All of her.’
‘Oh! Yes, of course, I’ll come and see her.’
Mrs Cochrane was the lady with severe asthma that I had put on a ventilator the day before. She had been quite difficult to intubate, and I had needed very high pressures, up to 65cm of water, to inflate her properly. I had tried all sorts of things in an attempt to lower this pressure but none of them had worked. And now she was ‘swelling up’! I guessed she was either very oedematous or had developed surgical emphysema.
When I got to the ward I found her looking like a Michelin man, and she was all crinkly to the touch because of minute bubbles of air in her subcutaneous fat. The swelling extended from the base of the nails of her toes right up to the line of her eyebrows, so that the features on her face had become quite unrecognisable. What on earth would her family think when they saw her? It would be difficult to convince them that she would get better from this gross appearance, and yet if we could only keep her going till the steroids relieved her bronchospasm all would probably be well. I wondered exactly where the hole was that was letting air escape from her respiratory tract into her tissues in this amazing fashion. She had been quite difficult to intubate; perhaps I had damaged the mucosa lining her trachea as I put the tube down. Still, high pressure like we were using could cause damage by itself without any pre-existing trauma. I had to break the spasm somehow. What about etherising her? I remembered the young girl David and Terence had etherised, without success, it was true, but this was different: Mrs Cochrane had not got air-trapping like that poor girl. It would certainly be worth a try.
This time I was determined to minimize the danger of using a flammable agent outside an electrically safe operating theatre suite. I would move her across the corridor to the acute dialysis room, but only after I had stripped it of all its electrical equipment, opened both the windows and put a big notice on the door warning people not to switch the lights on. I borrowed an anaesthetic machine from the ENT theatre, and brought it down in the lift to the ground floor. The dialysis room by this time looked starkly naked. It was something of a relief to wheel the big heavy machine into it to fill the void, and by the time I had pushed the patient on her bed across the corridor, the whole set up looked positively businesslike. I turned on 50% oxygen /50% nitrous oxide, and continued ventilating her by squeezing the bag of the anaesthetic machine. Her lungs were amazingly stiff, and the wheezing reverberated throughout the tubing. I wondered if ether really would do anything.
I slowly turned the ether on. As she was not breathing for herself, I could really only judge the depth of anaesthesia by her eye signs, and by watching her blood pressure too. I deliberately did not atropinise her before I began. Although the endotracheal tube was bypassing her mouth I guessed she would salivate nonetheless, and so it proved. But saliva was no bother, and if I could provoke any bronchial secretions I wanted these to be as wet as possible. I took her down till her pupils were central and widely dilated; her blood pressure remained fine. As she got deeper I was noticed that I could inflate her more easily than before, though the sound of the wheeze was not greatly altered at first. After ten minutes or so, I was able to convince not only myself, but also the nurse who was with me, that the bronchospasm was quieter, and possibly sounding wetter, though when I sucked down the tube I did not get any secretions. After another five minutes I turned the ether off, waited five minutes more, and took her back to the main ITU and reconnected her to the Cape ventilator. With same settings for rate and tidal volume, the maximum pressure was now only 40cm of water.
‘Let’s see what happens over the next few hours,’ I said. ‘Is her husband here yet?’
‘Yes, he’s in the waiting room
‘Has he seen her at all since she got this emphysema?’
‘No, not really. It will be an awful shock for him.’
‘I’ll go and talk to him. If he knows what she looks like before he sees her it won’t be quite so bad. Perhaps, if the pressure remains low, at least it may not get any worse; it might even start to get better.’
And that is just what happened. Within four days she was back to her normal self and we extubated her without a problem. The young registrar on the medical team was highly sceptical of the part played by the ether, but the consultant physician nodded wisely and said that he had heard before that ether was good for bronchospasm.
It was a lovely day. Cold, clear and crisp. The sort of day that made me consciously aware how good it was to be alive. I had slept well and had woken refreshed. As I left for work the dawn sky was streaked with crimson and yellow and blue, and as I topped the crest of Passage Rd the sun was a crimson globe hanging shamelessly above the rooftops of Westbury.
When I reached the hospital I parked outside the Medical School Unit and walked to the ‘day theatres’ as they were called. I nodded good morning to several of the people I passed on my way down the corridor and arrived at the theatre suite at twenty minutes to nine. Good, I thought, I've got time for a quick cup of coffee.
I opened the door to the changing room and at once was assailed by a strong smell of ether. What on earth was going on? I did not turn on the light for fear of sparks inside the switch and anyway there was a large skylight in the roof. The first thing I noticed was how unusually tidy the room was, theatre changing rooms in the hospital being renowned for the disgusting condition in which they were left by staff at the end of the working day - and often not much better at the start of the next. To-day it was different. In particular the boots on the floor were especially clean and bright.
There was no obvious source for the smell, yet it was all pervading. I looked in the small cupboards on the wall which were there so that people could lock up their valuables. Almost at once I found one that had a half full bottle of ether in it. Next to the bottle was an unlit pipe and a box of matches.
‘Good grief’, I cried out aloud to the empty room, ‘He's lucky that he hasn't blown himself up!’
I remembered with horror the time a fridge had exploded in the Medical School Unit; someone had been keeping some specimens in ether in the fridge and the vapour had leaked into the works with disastrous result, though luckily it was at the weekend and the building had been empty. Thank God nothing like that had happened here.
I opened the door and shouted down the corridor, ‘Jim, Jim, where are you?'
There was no answer. For a moment I wondered whether it was remotely possible that Jim was an ‘ether sniffer’. I did not think it was likely but why on earth was the bottle there when no-one actually used ether as an anaesthetic these days? Clearly it had been used for some purpose or other only a few minutes ago. But for what? I looked around the room again and then it dawned on me what had been happening:
Jim had been cleaning the surgeons' boots with ether! There they were, gleaming in the half light, like a row of snowmens' feet. That must be it.
I went out and searched the theatre suite for Jim. I found him in the coffee room.
‘Jim, I was looking for you.’
I felt just slightly anxious because I thought that I might look silly worrying about the ether. Perhaps I was overreacting. Still I would not be happy till I had had it out.
‘Jim, have you been cleaning the boots with ether?’
‘Yes. I always use ether. Colin showed me years ago how good it was and there really is nothing quite like it, you know.’
‘Well, I'm worried about it. I'm probably fussing but now we have stopped using explosive anaesthetic agents it would be pretty stupid if you blew us all up just trying to get the boots clean, now wouldn't it?’[1]
‘Yes, I suppose it would,’ he admitted reluctantly.
It was early in 1988 that ether became available in the UK only on a named patient basis, though this hardly mattered to us as there seemed no obvious reason why anyone should want to use it anyway - the age of ether was already long past.
In contrast, bottles of ethyl chloride are still common in our anaesthetic rooms. They are marked fine jet for local anaesthesia, though they are rarely used for this and certainly never for general anaesthesia. However, we still use ethyl chloride for testing the extent of anaesthesia after nerve blocks, especially spinals and epidurals. This relic of the past is the only occasion in modern anaesthetic practice that we allow a flammable agent to sully the air in our theatre suites; perhaps it is time we stopped.
We are no longer allowed to use ethyl chloride to test the height of our epidural blocks in the labour rooms, though I cannot remember exactly when, or from where, the edict came in the end. Surprisingly, it is still available in the anaesthetic rooms, both in the delivery suite and in main theatres. Nevertheless, these days when I want something cold to test a block I tear open a pre-injection swab and wipe it gently on the patient’s skin. The swab itself is saturated with 70% isopropyl alcohol. It works very well for a short while, but it soon gets dry, and anyway the cold feeling is not so intense as with ethyl chloride - nor is it so exciting!
There is still a dark bottle labelled ETHER in the anaesthetic office. It is kept inside the wooden case which contains the old pharmacy scales that I once planned to turn into a ‘Waller’s chloroform balance’[1], but never got around to doing. There is only a smidgen of ether in it - just enough to remind me of the smell, and to keep the memory of October 16th 1846 still alive.
NOTES
[1] When you consider how straightforward anaesthesia for circumcision is to-day, with the combination of a light general anaesthetic and a regional block, it is fascinating to read in a 1935 textbook[a]:
Circumcision usually causes a good deal of laryngeal spasm, especially in children. Don’t try to abolish this by deepening the anaesthesia. You won’t succeed unless you nearly kill the patient. Rub the lips, and if very severe ask the surgeon to stop a minute until the crowing becomes less. Beware of reflex syncope.
In the 1941 edition[b] the following comments were added:
Circumcision, especially in babies, is an operation which may give a certain amount of anxiety even to the most experienced anaesthetist.
and
Nitrous oxide and oxygen, supplemented by cyclopropane or ether, is most suitable, but if apparatus is not available for such agents, or the anaesthetist is not accustomed to dealing with very young children, open ether should be employed.
On the other side of the Atlantic, Guedel published his classic textbook Inhalational Anesthesia in 1937. He had this to say about operations on the prepuce:
The reflex activity in these operations is usually underestimated. ‘Just a little gas’ will not do. Anesthesia well into the lower first plane is necessary to control reflex movement for this surgery.
To-day when we block the afferent impulses from the operative site with a dorsal nerve block or a caudal block, we should understand that we are merely following the advice given by Crile in 1913. In his paper on anoci-association or shockless operation[c], for which he advocated the combination of general anaesthesia with local or regional anaesthesia, he wrote:
We must, therefore, conclude that, although ether anaesthesia produces unconsciousness, it is in reality a veneer, as it protects none of the brain cells against exhaustion from the trauma of surgical operations.
and -
If the field of operation is blocked, then only just enough ether need be given to hold unconsciousness, and so chemical damage may be reduced quantitatively to the minimum.
I wonder why it took us so long to learn the lesson!
[a] Ross JS. and Fairlie HP.. Handbook of Anaesthetics (4th Edition). Edinburgh: E & S Livingstone, 1935. [b] revised by Minnitt RJ. 1941.[c] Crile, George W. A kinetic theory of shock and is prevention by anoci-association (shockless operation). Lancet 1913; 2:7.
[1] This was fair comment as the orange capsule must have been Seconal (quinalbarbitone), and barbiturates are well known for their bitter taste. Although barbiturates were good sedatives they had no analgesic action, and patients who were given them were often restless postoperatively , unless adequate analgesia also was given. They went out of fashion once benzodiazepines became available.
[2] I realise now, of course, that it wasn't Balsa Wood Cement that I was smelling, but the ether with which I had been anaesthetised.
[3] Although surgeons to-day may favour rough foods after tonsillectomy, to help get rid of sloughs, I still remember how well the cold ice-cream soothed my throat.
[1] Even to-day ether, though obsolete as an anaesthetic, is widely used as a pharmaceutical and industrial solvent, and the latest edition of Martindale still mentions its use in removing plasters.
[1a] Still as it was then only 1949 we were many years ahead of Steptoe et al.
[1] though I have never seen bile salts injected intravenously to measure arm-tongue circulation time, in the late sixties we often used a weak solution of saccharin for this purpose in our pre-operative assessment of patients for cardiac surgery; if the time was over 90 seconds it was an indication of a very poor prognosis. One such patient, who preoperatively had pitting oedema from his feet to his nipple line, was given only 6.25mg (sic) of thiopentone at induction of his anaesthetic. This produced a marked effect. I am glad to say that he survived his aortic valve replacement, though he was on a ventilator for three weeks after the operation.
[2] I guess that to-day doxapram would do the same thing, though the dose should be kept small. Once in 1959 I injected 5ml of nikethamide, which has a similar action to doxapram, in order to produce an explosive cough and the patient said ‘I’ve gone blind’; she remained unable to see for two minutes, but then, to both our great reliefs, all was well once more. I read afterwards[a] that this injection should be ‘preceded if necessary by 0.1 - 0.2 g. of thiopentone’. I never tried this technique again. [a] Lee JA. Synopsis of Anaesthesia. 4th edition. Bristol: John Wright and Sons. 1959; 511.
[3] the administration of succinylcholine, when it produces fasciculations, gives the same sort of information in the anaesthetised patient.
[4] a minim is a sixtieth of a fluid drachm, which itself is 1/16th of a fluid ounce avoirdupois, though formerly , with apothecaries, it was 1/8th of an fl.oz - which is highly confusing.
[1] Over the years I have often told this story to our trainees. Imagine my surprise when one of them told it back to me some twenty years later as though it had happened to him. Quite a red face when I reminded him from where he had originally got the tale.
[2] Ethyl chloride is not actually much more potent than ether if the concentrations needed for anaesthesia are compared (MAC: ethyl chloride 2.0%; ether 1.9%), but because it is a gas at room temperature and is relatively non-irritating to inhale it is possible to breathe 100% ethyl chloride (i.e.50 x MAC). It is this that makes it potentially so dangerous, especially after a period of breath holding when the patient may already be hypoxic. On the other hand, used carefully it has proved to be safe. In 1955 Campbell and Smith[a] reported a series of 12,038 guillotine tonsillectomies under ethyl chloride anaesthesia without a single death, and concluded that the competent anaesthetist, who is aware of the dangers of ethyl chloride, can employ it safely. In 1959 Welsh[b] reported a series of 2,920 tonsillectomies in 1934 under ethyl chloride, and a further 35,000 tonsillectomies between 1947 and 1959, also without a death, though it is not clearly stated that all of these patients were given ethyl chloride. [a] Campbell JC and Smith DH. Guillotine tonsillectomy and curettage of adenoids under ethyl chloride anaesthesia. Brit. Med. J. 1951; 1451. [b] Welsh F. Death from tonsillectomy. Lancet 1959; i : 944.
[1] Named after a famous Guy’s physician, Thomas Addison (1793-1860), who 1849 described the condition of adrenal insufficiency.
[1] At this time it was quite normal for a patient to stay in hospital for two weeks, or even longer, after cholecystectomy; even a straightforward haemorrhoidectomy never went home until after the tenth day, for fear of secondary haemorrhage. It meant that the turnover in the surgical wards was very leisurely compared with to-day; the nurses used to have time to get to know the patients. The philosophy of post-operative care was very different in the fifties. In the words of one anaesthetist: uncomplicated cases are often allowed to sit up on the second or third day[a]. [a] A. Hamilton Bruce. In: Wilson Harlow F. ed. Modern Surgery for Nurses, 3rd edition. London: William Heinemann Ltd, 1954; page 480.
[2] Lotio Rubra - a solution of zinc sulphate, coloured with Amaranth; once a popular astringent.
[3] B.L.B (Boothby, Lovelace and Bulbulian) mask. Described in 1938, it had a small reservoir bag beneath the mask, and a variable proportion of air was admitted by rotating a sleeve which uncovered one, two or three holes. At low oxygen flows, say 3 L/min, there was considerable resistance to breathing, and also partial rebreathing[b] but at higher flows it acted rather like a Mapleson C system. [b] Langton Hewer C. Recent advances in anaesthesia, 7th edition, page 411. London: J & A Churchill, 1953.
[4] In this era there was, on every ward at Guy’s, a ‘stimulants tray’; this was an open tray with ampoules of Coramine (Nikethamide), a respiratory stimulant and general analeptic, and Methedrine (methylamphetamine), a vasopressor and central nervous system stimulant. If a patient collapsed the nurse would be expected to raise the legs, hold the chin, give oxygen, call for help and inject both these stimulant drugs intramuscularly. Occasionally a nurse on duty at night would open an ampoule of Methedrine and put a couple of drops into her midnight drink; it certainly helped her to stay awake during her long tour of duty, which was ten consecutive nights of twelve hours each, followed by three nights off. There was little general awareness in the community of the dangers of amphetamines. (see also chapter 11)
[5] It was not until 1960 that Kouwenhoven and his colleagues described their method of closed chest cardiac compression[c], though a description of artificial respiration in a case report in Hamilton Bailey’s Emergency Surgery 1935 sounds, when read today, remarkably like ECM!. Though Elisha, in the ninth century BC, resuscitated an apparently dead child by putting his mouth upon his mouth[d], artificial respiration in 1935 was still ‘indirect’, and relatively ineffective, and it was not until 1954 that it was shown that satisfactory gas exchange could be obtained by expired air resuscitation[e]. Despite this it was certainly not yet in the armamentarium of a houseman at Guy’s in 1958. [c] Kouwenhoven WB, Jude JR and Knickerbocker GG. Closed-chest cardiac massage. J. Amer. med. Ass. 1960; 173:1064. [d]. II Kings 5,34 [e] Elam JO, Brown ES and Elder JD. New Engl, J. Med. 1954; 250: 749.
[6] Edinburgh University Solution Of Lime, a popular and effective antiseptic lotion in days past, but currently under a cloud for causing destruction of healthy tissue.
[1] Scavenging of waste anaesthetic gases and vapours did not come into routine use until 1976. I joked at the time that anaesthetists would give up the job up once they were stopped from inhaling the vapours that hissed out of the expiratory valves, but I was wrong; it was a blessed relief! Within one week of scavenging being installed at Southmead I swore I would never work in a theatre again that did not have it. It is amazing that we had failed for 130 years to appreciate that there was a problem. (See also chapter 5/1956.) The attachments we needed in the Southmead district for the various anaesthetic machines were as follows: 70 Penlon Duct Expiratory Valves @ £9.96 each; 25 Penlon Papworth Safety Blocks @ £23.00 each, and 2 x 50ft lengths of light weight hosing - a total of £1302.90. Then there were the necessary wall outlet connections and the building and engineering works, whose cost I do not know. The overall cost throughout the country must have been enormous.
[1] Doughty A. A modification of the tongue-plate on the Boyle-Davis gag. Lancet 1957; i, 1074.
[1] Cole WH. Ethyl chloride as a gaseous anaesthetic. Anaesthesia.1956; XI, ii: 156.
[1] Denison Davies D. Re-anaesthetising cases of tonsillectomy and adenoidectomy because of persistent postoperative haemorrhage. Brit. J. Anaesth. 1964; 36: 244.
[2] Gorham AP. The role of the anaesthetist in the mangement of post-tonsillectomy in children. Anaesthesia 1964; 19: 565.
[1] There has only ever been one explosion involving ether at Southmead, as far as I am aware. This was not in an operating theatre, but in a research lab in the Medical School Unit in 1973. A sample of I-know-not-what had been kept dissolved in ether in a glass jar inside a fridge. The explosion was formidable, but luckily the building was empty at the time.
[1] Waller A.D. and Geets V. Brit Med J, 1903; 1, 1421. A splendid device for measuring and regulating the concentration of chloroform in an air/chloroform mixture, based on the difference in densities of air and chloroform vapour.
-
Waller's original balance. This considered in detail in Macintosh and Mushin's Physics for the Anaesthetist Blackwells 1946, from where this picture was taken.
email john@johnpowell.net